The Troublesome Cushing’s Syndrome
March 31, 2023 / General Health / By Hemopet https://hemopet.org/the-troublesome-cushings-syndrome/?utm_source=Klaviyo&utm_medium=campaign&_kx=qjTvDeFUAmu9T1-bVDHL1OrzQOTI-Sa8jw_Kf-MGhbY%3D.Ypvfhc

Cushing’s syndrome in dogs is complex, difficult to diagnose, and tricky to treat. Before we get into all of that, we need to review the mechanisms that may cause it.
The Physiological Mechanisms
The pituitary gland is located in the brain. The adrenal glands lie near the kidneys. The pituitary gland tells the adrenal glands what to do.
How does the pituitary gland do this? Well, it releases a chemical called adrenocorticotropic hormone (ACTH). ACTH then stimulates the adrenal glands to release another hormone called cortisol, which is commonly known as the “flight or fight” stress hormone.
When the Pituitary-Adrenal Connection Goes Awry
Pituitary-Dependent (PDH) – If the pituitary gland develops a tumor that is most often benign, it will overproduce and release more ACTH. This overproduction of ACTH causes the adrenal glands to overproduce and release more cortisol. Once the pituitary gland realizes that there is an excess of cortisol circulating in the body, it will then underproduce ACTH. This form of Cushing’s disease accounts for 80-85% of the cases in dogs.
Adrenal-Dependent (ADH) – More rarely, an adrenal gland can develop a tumor that may be cancerous. This, too, can cause the release of excessive amounts of cortisol and suppresses the release of ACTH.
Drug-Related – Oral or injectable prescription glucocorticoid steroids (a class of corticosteroids) can cause another form of Cushing’s syndrome, termed “iatrogenic Cushing’s syndrome” . They suppress the adrenal glands by adding extra cortisol to help fight skin or inflammatory conditions. When given in excessive amounts or over a long period of time, they can cause the iatrogenic Cushing’s syndrome.
Atypical Cushing’s – In dogs with atypical Cushing’s syndrome due to a problem with the pituitary gland or ADH , we can observe enlargement of the liver, liver pathology, and bilaterally enlarged adrenal glands are usually present. An increased endogenous ACTH level is seen, along with the usual clinical signs, blood work results and hair coat problems. The other adrenal gland can be atrophied (shrunken). There is a decreased endogenous ACTH level and the usual clinical signs, blood work results and hair coat problems. This form of Cushing’s syndrome can be more difficult to diagnose and measurement of 17-Hyroxy (17-OHP) progesterone before and after giving ACTH is often required (see more below).
Wait! I thought it was called Cushing’s disease?
Cushing’s disease is a form of Cushing’s syndrome and specifically refers to those with PDH tumors. Cushing’s syndrome is the general state of excessive levels of cortisol in the blood. In any event, the medical term for high levels of cortisol circulating in the blood is hyperadrenocorticism.
Signs of Cushing’s Syndrome
The most telltale sign of Cushing’s syndrome is a pot-bellied appearance. Additional signs are panting, dark spots, bladder infections, thin hair and/or skin, fat pads, excessive drinking and eating, and excessive amounts of calcium deposits in the skin (calcinosis cutis/skin mineralization).
This constellation of Cushing’s signs are called Cushingoid.
Diagnosing Cushing’s Syndrome
We can analogize the current diagnostics for Cushing’s syndrome with shopping for a couch. Have you ever gone couch shopping and you like certain features from different couches, but nothing’s perfect? For instance, you like the cushions on one model, but detest the armrests? Or, you like the armrests on another, but it has an upholstered skirt that you don’t like? Let’s not even get into the length, height, depth, fabric, patterns or colors!
Anyway, Cushing’s diagnostics are similar to the variety of couches: there are a lot of options, nothing’s perfect and all of it costs a bundle. But, unlike a couch, you cannot customize the diagnostics.
This is not to negate Cushing’s testing. Indeed, you need to have positive confirmation of Cushing’s syndrome and the location of the problem (pituitary or adrenal) before medicating.
Urinary Cortisol to Creatinine Ratio (UCCR) – This test is used as a pre-screening tool to rule out Cushing’s syndrome by measuring the first morning urine at home. However, stress can cause this number to fluctuate greatly, which is why you need to collect your pet’s urine at home (one teaspoon is enough in a clean plastic dish) when he first gets up and has not exercised, and then take it into your veterinarian to run this test. Even if it is negative, and the veterinarian still highly suspects Cushing’s syndrome, further testing is necessary.
Ultrasound – An abdominal ultrasound helps by pointing us in the right direction. With PDH, both adrenal glands are abnormally enlarged. Whereas ADH, only one adrenal gland is enlarged and the other is small or atrophied.
ACTH Stimulation Test – If any dog has been given steroids in the past, this is the test experts want to use to diagnose iatrogenic Cushing’s syndrome. However, ACTH stimulation has a sensitivity of only 60%-85% (percentage of true positives), and a specificity 60%-93% (percentage of true false negatives). Additionally, it does not indicate the location causing the Cushing’s syndrome.
If this is the chosen test, it is wise to concurrently analyze 17-Hydroxyprogesterone (17-OHP) concentrations in response to ACTH administration. Dogs with atypical Cushing’s disease have an exaggerated 17-OHP response to ACTH. Other dogs with Cushing’s syndrome could have deranged steroid production pathways, such that certain steroid precursors may be abnormally increased and responsible for the presenting clinical signs, whereas cortisol concentrations are normal.
By the way, diagnosis of atypical Cushing’s disease may also include measurement of: androstenedione, estradiol, progesterone and aldosterone.
Low Dose Dexamethasone Suppression Test (LDDS) – This is considered the gold standard for testing for Cushing’s syndrome at this time unless iatrogenic Cushing’s disease is suspected. It can distinguish between PDH and ADH. The sensitivity is good at 95%, but the specificity is poor and only 50%-75%.
Endogenous ACTH (eACTH) – Endogenous ACTH should not be used to diagnose Cushing’s disease, but will help with location and secondary confirmation. The sample has to be prepared properly at the veterinarian’s office to ensure stability, then frozen, and sent frozen to a veterinary reference laboratory. Due to all of these handling factors, it is really not an ideal test unless the blood collection is at a research institution.
Zomedica has developed an in-house, point-of-care diagnostic machine that measures eACTH using bulk acoustic wave technology. (This is not an endorsement; we simply want you to know your options.) An LDDS test or ACTH will still need to be conducted.
Options to Treat Cushing’s Syndrome
If Cushing’s syndrome is confirmed, veterinarians have only a handful of treatment options. In fact, many veterinarians choose not to medicate for the disease based on bloodwork, other currently prescribed medications, additional conditions, and potential side effects of the Cushing’s disease medications.
Surgery – If it is ADH, surgical removal of the tumor is possible but can be very difficult, especially if it has spread. However, due to the complexity of removal, most cases are treated with medication.
Trilostane (Vetoryl) – At this time, this is the only prescription medication approved by the Food and Drug Administration (FDA) to treat both PDH and ADH. Trilostane works by stopping the production of cortisol in the adrenal glands. However, it should not be given to a dog that takes certain medications for heart disease, is pregnant, and/or has kidney or liver disease. Additionally, the ACTH stimulation test is preferred to monitor trilostane therapy. Return of clinical signs of Cushing’s disease can occur in some dogs while still on trilostane.
Common side effects are poor or reduced appetite, vomiting, lack of energy, diarrhea, and weakness. More serious (but considered rare) side effects include bloody diarrhea, collapse, severe sodium/potassium imbalance, and destruction of the adrenal gland that may result in death.
Selegiline (Anipryl) – Selegiline is an monoamine oxidase inhibitor (MAOI), and is also FDA approved, but only for uncomplicated PDH. It should not be given to dogs that take other MAOIs, meperidine, tramadol, tricyclic antidepressants, selective serotonin reuptake inhibitors, or alpha-2 agonists.
Side effects include vomiting, diarrhea, restlessness, disorientation/confusion, aggression, repetitive movements, tiredness, drooling, itchiness, licking, trembling, and lack of appetite. Rare, but serious side effects, include deafness and panting more than usual.
Mitotane (Lysodren) – Mitotane is a human chemotherapy drug that veterinarians can prescribe “off-label” to treat Cushing’s disease. It works by destroying the layers of the adrenal gland that produce cortisol. It should be used cautiously in pets with diabetes mellitus or kidney or liver disease. The following medications should be used with caution when given with mitotane: central nervous system (CNS) depressant drugs, fentanyl, insulin, midazolam, phenobarbital, selegiline, spironolactone, or warfarin.
Common side effects are decreased appetite, vomiting and diarrhea. Other side effects include lethargy, incoordination, weakness, or yellowing of the skin, gums, or whites of the eyes.
Regular monitoring of cortisol levels is required.
Melatonin – The enzymes that are typically elevated in HAC are inhibited by melatonin. Also, in dogs with adrenal disease treated with melatonin, repeat adrenal steroid panels show that cortisol levels are consistently reduced. Melatonin treatment for cases of mild to moderate canine adrenal disease can be effective, and particularly in cases where adrenal sex steroids are increased.
Melatonin plus phytoestrogens – Melatonin given in combination with phytoestrogens (isoflavones, lignans, and genistein) is known to inhibit adrenal steroid production. Combinations of melatonin and phytoestrogens, especially the SDG flax hull or HMR Norwegian spruce lignans have proven increased efficacy in treating these conditions.
References
“Adrenal Function Testing.” The College of Veterinary Medicine at Michigan State University, Michigan State University, https://cvm.msu.edu/vdl/laboratory-sections/endocrinology/adrenal-function-testing.
Behrend, E N et al. “Diagnosis of spontaneous canine hyperadrenocorticism: 2012 ACVIM consensus statement (small animal).” Journal of veterinary internal medicine vol. 27,6 (2013): 1292-304. doi:10.1111/jvim.12192, https://onlinelibrary.wiley.com/doi/full/10.1111/jvim.12192.
Dodds, W. Jean. “Diagnosing Atypical Cushing’s Disease/Syndrome in Dogs.” Dr. Jean Dodds’ Pet Health Resource, Tumblr, 17 Apr. 2016, https://drjeandoddspethealthresource.tumblr.com/post/142960916541/atypical-cushings-dog#.Y6CxAXbMLIW.
“Treating Cushing’s Disease in Dogs.” U.S. Food and Drug Administration, FDA, 8 July 2021, https://www.fda.gov/consumers/consumer-updates/treating-cushings-disease-dogs.
Jonathan the Tortoise, The World’s Oldest Animal, Turns 190
DEC 8, 2022 from Twisted Sifter https://twistedsifter.com/2022/12/jonathan-the-tortoise-the-worlds-oldest-animal-turns-190/?utm_source=040523-FP-WIMP-FB&utm_medium=WIMP-FB&utm_campaign=WIMP-FB&utm_content=2022%2F12%2Fjonathan-the-tortoise-the-worlds-oldest-animal-turns-190
Happy 190th birthday to the oldest animal, and oldest tortoise, in the human record.
His name is Jonathan and he was given the title by the Guinness World Records, after confirming that he hatched in 1832 based on photographic records.

According to The Guardian, governor of the British overseas territory Nigel Phillips declared Jonathan’s birthday to be December 4, 1832. The tortoise was then feted like royalty, including a three-day celebration at the governor’s residence on the island of St Helena in the South Atlantic and a reptile-friendly cake.
The only official record used to prove Jonathan’s age was an old photograph that shows the turtle arrived on the island in 1882. In the photo, he appears to be fully mature and estimated to be at least 50 years old at that time, making his birth around 1832.
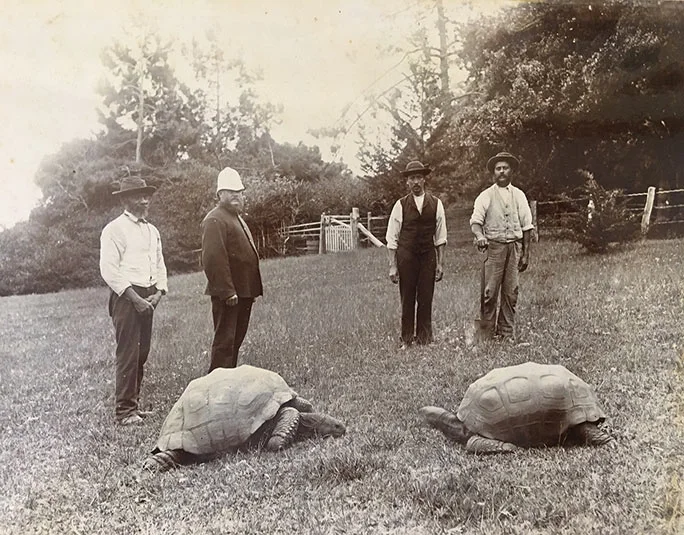
Impressive as his new title is, the birthday boy isn’t as spry as he once was. Jonathan is blind and has lost his sense of smell, but he still has a healthy appetite. Apparently, his favorite foods are lettuce hearts and bananas. Here’s to Jonathan and 190 more!
A dog died after getting bird flu in Canada. Here’s how to keep your pets safe.
See the video here: https://www.usatoday.com/story/news/health/2023/04/05/dog-dies-bird-flu-how-to-keep-pets-safe/11607516002/
Adrianna Rodriguez USA TODAY
A pet dog has died after testing positive for the highly contagious bird flu in Ontario, Canada, health officials said this week.
The Canadian Food Inspection Agency said the dog tested positive for the virus on Saturday after chewing on a wild goose. The dog subsequently developed clinical signs and died.
While further testing is underway, a necropsy showed its respiratory system may have been compromised by the virus, according to Tuesday’s statement.
Canadian health officials say it’s the first case of its kind reported in the country. The American Veterinary Medical Association says only a few cases of bird flu in cats or dogs have been reported worldwide, with none occurring in the United States.While the U.S. Department of Agriculture hasn’t reported any cases among pets, the agency has found cases in other mammals like skunks, raccoons, mountain lions, bears and foxes. Canadian health officials say it’s the first case of its kind reported in the country. The American Veterinary Medical Association says only a few cases of bird flu in cats or dogs have been reported worldwide, with none occurring in the United States.
While the U.S. Department of Agriculture hasn’t reported any cases among pets, the agency has found cases in other mammals like skunks, raccoons, mountain lions, bears and foxes.
How to keep your pet safe from bird flu
Canadian and U.S. health officials say pets’ risk of contracting and dying from bird flu appears to be very low – but not zero.
Here’s what you can do to keep your pet safe from bird flu:
►Don’t feed pets, including dogs or cats, raw meat from game birds or poultry.
►Keep pets away from dead wild birds found outside.
►Contact a veterinarian if your pet develops symptoms including fever, lethargy, lack of appetite, difficulty breathing, tremors or seizures, or conjunctivitis.
“Words Matter” – The Whole Dog Journal
Why the language you use makes a difference in your relationship with your dog – and perhaps even the success of your training program.
By Pat Miller, CBCC-KA, CPDT-KA

I’ve been training dogs professionally for 27 years, but I don’t use “commands” for this purpose, I use “cues.” What difference does it make? A lot!
The definition of command is “an authoritative order.” Even when we use gentle training methods, if we think “commands,” our brains connect to the authoritative definition and we are likely speak in a louder, harsher (commanding!) tone of voice. In contrast, a cue is an invitation to perform a behavior for which your dog can be reinforced with a treat, play, praise, or the opportunity to perform a behavior the dog enjoys. We are far more likely to speak softly and gently when we use “cues.”
Words to avoid
“Command” is just one of many words that we force-free trainers avoid. Here are others that interfere with the message of kindness and mutual respect we want to send to our dogs:
- “It.” This word is used to refer to non-living objects. Dogs (and other animals) are living, thinking, feeling beings. Use he, she, him, and her rather than “it” when referring to a dog. When you acknowledge the sentience of non-human animals, you’re likely to treat them better.
- “Breaking.” Breaking evokes force, and we’re not “breaking” anything, we’re “training” – so we use housetraining (not housebreaking) and say we are training desirable behaviors (not breaking bad habits).
- “Obedience.” We want a partnership with our dogs – a happy willingness to offer behaviors we ask for, not their submission to our authority. That’s why we offer good manners training or family dog training rather than “obedience classes.”
- “Make.” We don’t “make” our dogs do things. “Make” suggests force and coercion. Instead, we ask our dogs for certain behaviors, invite them, help them, and encourage them.
- “Bad.” Dogs aren’t bad and they don’t do bad things – though occasionally they may do something inappropriate. When we think of them as bad, we give ourselves tacit permission to punish them. But when we frame their behavior as “inappropriate,” we’re more likely to think in terms of management and teaching appropriate behaviors rather than punishment.
- More pejoratives. I cringe when someone refers to a dog as stupid, stubborn, disobedient, or any other negative adjectives, placing the blame for any unwanted behavior directly on the dog’s shoulders. When a dog doesn’t do what you ask, it’s because she can’t for some reason: she doesn’t understand, she’s too stressed, was distracted, didn’t hear you, is in pain or otherwise physically unable, you haven’t made the consequence of the behavior reinforcing enough, or you haven’t generalized it well (you haven’t trained her!). Figure out why she can’t do it and then help her succeed.
Respectful language
Think carefully about the words you and/or your instructor use to discuss training and your dog. Philosopher and cognitive scientist Daniel Dennett suggests that language lays down the tracks upon which thoughts can travel. Your words connect to your thoughts and influence your behavior. If your words align with your philosophy of creating a kind and nurturing relationship with your dog based on mutual trust and respect, you’re likely to behave accordingly – and you and your dog will be well on your way to achieving that pinnacle.
WDJ’s Training Editor Pat Miller, CBCC-KA, CPDT-KA, grew up in a family that was blessed with lots of animal companions: dogs, cats, horses, rabbits, goats, and more, and has maintained that model ever since. She spent the first 20 years of her professional life working at the Marin Humane Society in Marin County, California, for most of that time as a humane officer and director of operations. She continually studied the art and science of dog training and behavior during that time, and in 1996, left MHS to start her own training and behavior business, Peaceable Paws. Pat has earned a number of titles from various training organizations, including Certified Behavior Consultant Canine-Knowledge Assessed (CBCC-KA) and Certified Professional Dog Trainer – Knowledge Assessed (CPDT-KA). She also founded Peaceable Paws Academies for teaching and credentialing dog training and behavior professionals, who can earn “Pat Miller Certified Trainer” certifications. She and her husband Paul and an ever-changing number of dogs, horses, and other animal companions live on their 80-acre farm in Fairplay, Maryland.
Giardiasis and Coccidiosis in Puppies
from: The Whole Dog Journal
How Much Food to Feed a Dog
How Much Food to Feed a Dog
Feeding guidelines for dogs—including how much to feed a puppy—are little more than a ballpark reference. Here’s how to feed your dog properly.
Recent News Report on Mixed-Breed Dog DNA Tests
From the WHOLE DOG JOURNAL by Nancy Kerns Published: March 9, 2023
On March 4, CBC News (Canada’s publicly owned news and information service) ran a television and online report about an investigation of four companies that offer dog DNA tests that purport to identify the breeds in mixed-breed dogs. Within a day, practically everyone I know was posting links to the online report with comments like, “I knew those tests were bunk!”
In the past 15-plus years that they’ve been available, I’ve been skeptical of the ability of these commercial testing products myself. However, I will say that, in my experience – and that of the CBC report – two companies in particular seem to provide results that are at least in the ballpark of possibility for the most common dog breeds found in North America. And one company seems to have a pretty good handle on identifying the origin of mixed breed dogs from other parts of the world. My response to the report, though, takes in a few details that many commenters seemed to miss.
The CBC sent DNA samples for four individuals to four different companies that offer mixed-breed dog DNA tests: Accu-Metrics, DNA My Dog, Embark, and Wisdom Panel. But they picked odd (in my opinion) candidates to use for the tests: A human, a purebred Great Dane, a mixed-breed dog from Turkey, and a mixed-breed dog from Kuwait.
As far as the human sample was concerned: I was pleased to learn that Embark and Wisdom Panel immediately sussed out that no dog DNA was present in the sample. And was not terrifically surprised when Accu-Metrics and DNA My Dog returned various dog-breed mixes in their results for the human sample. (Before seeing this report, I had never heard of Accu-Metrics before, and, a long time ago, received similarly incredible results of a test from DNA My Dog.)
The latter two companies also failed to accurately identify the purebred Great Dane. Results from DNA MY Dog suggested the dog was mostly Great Dane, but also 10% -25% Staffordshire Bull Terrier. Accu-Metrics returned the breed that the CBC suggested on its submission form that the dog most resembled: a Chihuahua! I don’t see any need to further discuss any results – or ever recommend the services from – either of those two companies.
Both Embark and Wisdom Panel correctly identified the Great Dane as 100% Great Dane.
Mixed-Breed Dogs from Other Continents
I so wish that CBC had used mixed-breed dogs from North America as their last two “test dogs,” because there are likely to be very few representatives of the most common purebreds dogs on other continents in Embark’s and Wisdom Panel’s databases. The most common (or likely) mixed-breed dogs on the streets in Turkey and Kuwait are not likely to be the breeds that are most common (or likely candidates) mixed-breed dogs found in Canada or the U.S.
Wisdom Panel identified the breed mix for the Turkish dog as Segugio Italiano, Chihuahua, Anatolian Shepherd, German Shepherd, and Estrela Mountain Dog. Without information as to how common those dog breeds are found in Turkey, it’s impossible to know how accurate this might be. To its credit, Embark identified the breed mix of the same dog as 100% West Asian Village Dog – meaning they were able to pinpoint the mixed-breed dog’s geographical origins. I’d call that a home run!
Similarly, Embark identified the dog from Kuwait as 100% Arabian Village Dog – again, at least accurately identifying the dog’s geographical place of origin. (Kuwait is also located in West Asia, but also at the northern edge of Eastern Arabia.) Wisdom Panel identified the dog as being a mix of American Pit Bull Terrier, Chihuahua, German Shepherd, Segugio Italiano, and Xoloitzcuintle.
Comparing Embark and Wisdom Panel, the two leaders
I’m a little dubious about the idea that these two foreign-born dogs could share three breeds in their Wisdom Panel results (Chihuahua, German Shepherd, Segugio Italiano), so I’m rather more impressed with Embark’s performance here. However, I’d want to compare the results from these two companies on more prosaic mixed breed dogs from this continent before dismissing Wisdom Panel altogether. In our past comparisons, using my two mixed-breed dogs Otto and Woody, the results were pretty darn close.
Otto’s DNA Test Results:


Woody’s DNA Test Results:


Back when I was still fostering Boone, my 1-year-old adolescent dog, I ordered a DNA test kit from Wisdom Panel, and these were the results:

But I think I am going to go ahead and order a test kit from Embark, to compare these results. I have a feeling, based on the CBC report, that I might invest a little more confidence in Embark’s results, but I’ll let you know!
Nancy Kerns has edited horse and dog magazines since graduating the San Francisco State University Journalism program in 1990. The founding editor of Whole Dog Journal in 1998, Nancy regularly attends cutting-edge dog-training conferences including those for the International Association of Animal Behavior Consultants, Pet Professional Guild, Association of Professional Dog Trainers, and Clicker Expo. To stay on top of industry developments, she also attends pet industry trade shows such as Global Pet and SuperZoo, educational conferences of the American Holistic Veterinary Medical Association and Pet Food Industry’s Pet Food Forum. As a regular volunteer for her local animal shelter, the Northwest SPCA in Oroville, CA, she fosters large litters of puppies and helps train wayward adolescent dogs in order to increase their chances of adoption. Nancy shares her life with her husband and two canine alumni of the NWSPCA, mixed-breed Otto (whose adorably fuzzy visage was incorporated into WDJ’s masthead some years ago) and Pit/Lab-mix Woody.
Current Issue
Download The Full April 2023 Issue PDF
Resources

© Belvoir Media Group, LLC. All rights reserved.
March is Pet Poison Prevention Month
What to Do If Your Dog Eats Marijuana (Edibles, Weed, Vape Cartridges, etc.)
The amount and type of THC-containing product consumed will determine the seriousness of this event for your dog, and dictate the level of your emergency response.
By Jennifer Bailey, DVM for WHOLE DOG JOURNAL Published: January 15, 2023
Recreational marijuana has become legalized in 21 states and medical marijuana can be prescribed in 37 states. As marijuana becomes more widely available, people are looking for ways to partake of this drug without having to smoke it. This has created a market for marijuana “edibles,” also known as cannabis edibles.
Cannabis edibles are products that contain the psychoactive component of marijuana called delta-9 tetrahydrocannabinol (THC). A variety of products are available as cannabis edibles, including gummies and other candies, mints, chocolates and chocolate bars, beverages, potato chips, and baked goods such as brownies and cookies. Unfortunately, many of these sweet or savory options are also attractive to our dogs. While we may have more self-control regarding how many edibles we consume at one time, dogs are more likely to ingest an entire package of any edibles they can reach because they taste delicious.
Symptoms of THC Ingestion in Dogs
Ingestion of small to moderate amounts of THC may cause the following signs in dogs: listlessness, incoordination when walking, falling over when standing, dilated pupils, slow heart rate, dribbling urine, and an exaggerated response to light, touch, and sound. Dogs who have ingested large amounts of THC may have slow breathing, low blood pressure, and may exhibit seizures or become comatose.
What to Do If Your Dog Ate a Cannabis Product
If you observe your dog ingesting cannabis edibles, take him to your veterinarian or the closest animal emergency or urgent care facility immediately. If the ingestion occurred within 30 minutes of arrival at the hospital and your dog is not showing clinical signs of THC ingestion, then the veterinary staff may induce vomiting.
If it has been more than 30 minutes since ingestion of the edible or your dog is showing signs of listlessness, then vomiting will likely not be induced. This is because THC has an anti-emetic effect; it can suppress vomiting. If your dog is already listless, causing your dog to vomit in this depressed state can lead to aspiration pneumonia. Activated charcoal may be administered to absorb THC and minimize the effect it has on your dog’s body. If the edible contains chocolate or xylitol, then additional treatments may be necessary.
What If You Are Not Sure If Your Dog Ate a Cannabis Product?
If your dog is exhibiting signs of THC ingestion, but you did not witness or find evidence of this, have your dog evaluated by a veterinarian immediately. Be honest about what you have in the home, including any products containing THC, prescription sedatives, vape cartridges (including nicotine), and illicit drugs. Children, seniors, and roommates living in the home may not always be forthcoming about what they are storing in their bedrooms, so be firm yet gentle when inquiring about the presence of these products. The veterinary staff wants only to help your dog. They are not interested in contacting authorities about anything illegal in your home.
The clinical signs of THC ingestion look similar to the signs associated with ingestion of other sedatives, nicotine, and antifreeze. There is an antidote for antifreeze ingestion and without this intervention, this toxicity is always fatal. Your veterinarian may want to complete additional testing to rule out other causes for your dog’s clinical signs so that the appropriate treatment plan is initiated.
Although there is a urine test for THC available for use in people, this test is not always accurate in dogs. Dogs metabolize THC differently than people, so there is a high rate of false negatives with this test. However, a positive test for THC is almost always compatible with THC ingestion.
If ingestion of THC is suspected and the potential source has been identified, the veterinary team may contact animal poison control for further guidance regarding treatment. There are a number of variables that can alter how THC affects your dog. These variables include how much was ingested, your dog’s weight and concurrent medical conditions, any medications or supplements your dog may be taking, how the THC was infused into the product, and if the edible contains chocolate or xylitol.
Brownies, chocolates, and chocolate bars containing THC add another dimension to your dog’s toxicity: ingestion of theobromine and caffeine. Both of these are contained in chocolate and are toxic to your dog. Just like with THC, the type of chocolate (such as dark or milk chocolate), the amount ingested and the weight of your dog dictate the danger level and recommended treatment. (See “What to Do If Your Dog Eats Chocolate.”)
Gummies, mints, other THC edible candies and even baked goods may contain xylitol, an artificial sweetener that is toxic to dogs. Even tiny doses of xylitol are toxic to dogs, so it is important to know if any edibles your dog may have consumed contain xylitol.
Treatment for Cannabis Ingestion
Most mild cases of THC ingestion can be treated successfully at home by keeping your dog in a safe, quiet room where he cannot fall down the stairs or be exposed to excessive light or sound. Moderate cases of THC ingestion may require hospitalization with intravenous fluids, monitoring of heart rate and blood pressure, and medications to support the cardiovascular system and treat neurologic signs. Ingestion of high doses of THC will require hospitalization and may necessitate the administration of intralipids. Intralipids bind to THC so that it can be excreted safely from the body.
Ingested THC is fat soluble and is readily stored in body fat. Therefore, it can take anywhere from 12 to 36 hours for your dog’s clinical signs to resolve after ingesting a cannabis edible.
If you use cannabis products, store them in a locked drawer or cabinet. Dogs are clever and some can open drawers and cabinets, but I have yet to meet one that can insert a key in a lock!
Dr. Jennifer Bailey is a 2012 graduate of the Western University of Health Sciences College of Veterinary Medicine. She is an emergency and urgent care veterinarian at an emergency and specialty practice in Syracuse, New York.
PURINA PRO PLAN RECALL

Nestlé Purina Petcare Company Voluntarily Recalls Purina Pro Plan Veterinary Diets El Elemental Dry Dog Food in the U.S. Due to Potentially Elevated Vitamin D
Nestlé Purina PetCare Company is voluntarily recalling select lots of Purina Pro Plan Veterinary Diets EL Elemental (PPVD EL) prescription dry dog food due to potentially elevated levels of vitamin D. Vitamin D is an essential nutrient for dogs; however, ingestion of elevated levels can lead to health issues depending on the level of vitamin D and the length of exposure. Vitamin D toxicity may include vomiting, loss of appetite, increased thirst, increased urination, and excessive drooling to renal (kidney) dysfunction.
Purina is taking this action after receiving two contacts about two separate confirmed cases of a dog exhibiting signs of vitamin D toxicity after consuming the diet, to date. Once taken off the diet, each of these dogs recovered.
The affected dry dog food was distributed throughout the United States by prescription only through veterinary clinics, Purina Vet Direct, Purina for Professionals, and other select retailers with the ability to validate a prescription.
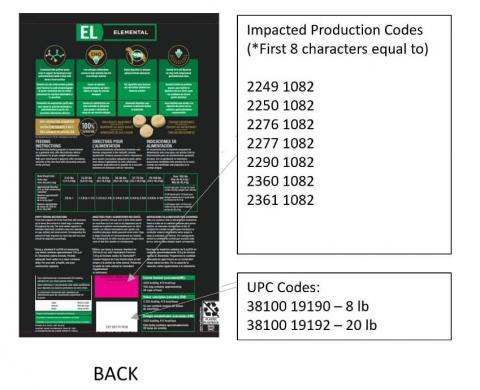
Bags of PPVD EL with the UPC Code and Production Code below should be immediately discarded.
| Product | UPC Code | Production Code (*First 8 characters equal to) |
|---|---|---|
| Purina Pro Plan Veterinary Diets EL Elemental (PPVD EL) 8 lb and 20 lb bags | 38100 19190 – 8 lb 38100 19192 – 20 lb | 2249 1082 2250 1082 2276 1082 2277 1082 2290 1082 2360 1082 2361 1082 |
Pet owners who purchased bags of the product listed above are asked to immediately stop feeding and throw it away in a container where no other animals, including wildlife, can get to it. If signs such as weight loss, excessive drooling, vomiting, loss of appetite or increased thirst or urination have occurred in their dog while eating this diet, pet owners should contact their veterinarian.
No other Purina pet care products are affected.
Veterinary and other retail partners should remove and destroy the affected product from their inventory.
We apologize to pet owners and veterinarians for any concerns or inconvenience this situation has caused. As pet experts and pet owners ourselves, the health and well-being of pets is our top priority.
Please contact our team directly Monday – Saturday, 8am – 5pm CST at 1-800-345-5678 or via email at https://www.purina.com/contact- usExternal Link Disclaimer for questions or assistance in getting a refund.
Company Contact Information
Consumers:Purina 1-800-345-5678