Can Your Dog Settle Down on Cue?

| An important skill for impulse control is the ability to settle down in the face of excitement. There is a lot of value in “installing an off switch” in your dog! It translates into the ability to get your dog to settle on cue even when she is very excited. This is especially useful when you want to let your dog know that an activity or a game has ended. Some high-energy dogs simply don’t know when to stop, and they can keep going long after you’ve already tired of the activity. An effective way to turn off activity in an action-loving dog is to teach an “all done” cue. This one doesn’t specifically tell the dog what to do – it just signals to her that the activity is over. Use any cue that makes sense to you, such as “All done!” or “That’s all!”. The sooner you “install” an off-switch in your high-energy, activity-persistent dog, the better. Remember, the longer the reinforcement history for persistence, the more persistent she’ll be. 1. Start teaching this behavior by engaging in your dog’s favorite activity – say, fetching a ball. After a reasonable period of fetch time, say “All done!” and put the ball away, out of sight, perhaps in a nearby cupboard. 2. Give your dog a reasonable alternative that she can do by herself, such as emptying a stuffed Kong. 3. Go sit down and occupy yourself with something, such as reading a book, watching TV, or web-surfing. 4. Ignore any attempts on your dog’s behalf to re-engage you, such as going to the cupboard and barking, or bringing you a different toy. 5. Don’t even repeat your off-switch cue, just ignore her. 6. Warn all other nearby humans to similarly ignore her attempts to engage them in activity when she’s been given the “All done” cue. Be prepared to quietly (so as not to get her aroused again) praise her when she finally lies down and starts to chew on the stuffed Kong. 7. Use your off-switch cue every time you end a play session with her favorite activity, and don’t give in if she persists. The more consistent you are, the sooner you will see her resign herself to the fact that the fun really is over when you say it is. If your dog does not like to fetch a ball, try another similar “get excited and settle” game such as running around together with a stop and settle. Or, play tug-and-drop, or try playing with a flirt pole (a toy on the end of a rope, which is fastened to a pole) to get your dog running, and then incorporate the stop and settle.Looking for more ways to teach your high-energy dog to chill out and relax? With Calm Down Rover from Whole Dog Journal, you’ll have instant access to vital training techniques. We all owe it to our dogs to understand why they act the way they do.www.whole-dog-journal.com |
Introducing Petfundr!
PetFundr provides crowdfunding for your pet’s urgent, acute or chronic care needs. With PetFundr, you can do it fast, reliably and for FREE!

Boydston Senior Grant Helps Lulu Find New Lease on Her Life

Noreen Sturges, who lost her 15-year-old canine companion Papillon last year, found a replacement a few months ago in Lulu, a female Maltese. “Lulu was rather matted, had a hacking cough and needed care and lots of love,” Noreen said.
Lulu had belonged to a family that was no longer able to provide her with the care and attention she needed. When Lulu was brought to Noreen’s home, “it was love at first sight,” she said.
Noreen hired a groomer to attend to Lulu’s matted hair. After the grooming, Noreen took Lulu to Monarch Veterinary Hospital in Laguna Niguel not far from her home.
Dr. Kelly Alcala examined her and found some serious dental issues that would require surgery and the extraction of some teeth. Lulu also had a hacking cough – “not like she would have had with a cold,” Noreen said. Dr. Alcala told her that she thought decay from the dog’s teeth was getting into her digestive system and probably causing the cough, Noreen said.
The doctor suggested that Noreen apply for a Boydston Grant to help pay for Lulu’s treatment and surgery. A grant of $500 was approved and Dr. Alacala did the surgery. The dog is now thriving, Noreen said, and the hacking cough is gone.
Lulu is eating her new diet voraciously. “And she’s a love!” Noreen said. “Everything’s good now.” The dog, she said, “is running around – up and down the stairs and all over the place.
“I didn’t think I could ever love a dog as much as my Papillon, “but I just love Lulu.”
She added that she is grateful for the help provided by her Boydston grant and the matching sum from Monarch Hospital, as well as for the work of Dr. Alcala. “I just love her, too,” she said.
Noreen said that she and Lulu “are having a lovely time together. She is quite a companion.”
Spooky Gets Great Christmas With Boydston Fund Assist

Spooky, a beautiful black and white, mostly wild cat, came into the Sparacinos’ lives in October, 2008.
“I thought she was an angel who had descended on us,” Donna Sparacino said. “She would drop down from the roof onto our deck and then come through our sliding glass doors into the main area of our two-level apartment and have lunch with our Maine Coon cat.
“But when my husband Terrell and I would come home from work, she wouldn’t let us get close. She would zip out the sliding door, jump up on the roof and she’d be gone. She was very skittish.” (The Sparacinos left their patio door ajar when they were gone so Dougal, the Maine Coon, could go out on the patio.)
Spooky’s route to the roof was up a short flight of steps near the San Clemente unit’s front door, then a leap of about five feet to the eave of the roof and a short walk to a spot on the roof above the patio.
“Dougal adopted Spooky before we did,” Donna said. “I couldn’t tell you how many times we’d come home and she was in the house until one day I saw her being groomed by Dougal. And I thought, ‘Whoa. I guess there’s a connection going on here.’”
In December, 2008, Donna and Terrell found Spooky near their front door with a dime-sized hole in her back from a BB gun pellet. They took her to Dr. Kelly Alcala, who was working at Canyon Animal Hospital in Laguna Beach. She treated the wound but the pellet remains lodged in the cat’s lung.
That brought Spooky into the Sparacino apartment permanently. “We knew we had to keep her off the streets and inside our home,” Donna said.
Dougal died in November but another male cat, Teddy, had been added to the household about a year ago. When Dr. Alcala moved to Monarch Veterinary Hospital in Laguna Niguel, Donna and her cats followed her there.
“My description of her, No. 1, is compassion,” Donna said. “You find a vet that feels what you feel and they just know. And it’s all for the best interest of the animal.”
Donna took Spooky to see Dr. Alcala for her wellness checkup last September at Monarch Hospital. The veterinarian recommended dental treatment for inflamed gums and heavy tartar.
But, Donna said, “things are kind of tight around here. I’m on my fixed social security income. And Terrell had lost his job in March of 2020. We thought maybe we could let the senior [blood] panel go – part of the wellness checkup – but Dr. Alcala said: ‘You really need to have the blood panel before you get any work done on the teeth.’ We wanted to wait a little bit before doing the teeth.
“But she said, ‘You know what? Because you’re seniors on a fixed income, and all the things that are going on [such as Covid], there’s a possibility you can get some help.’”
The doctor suggested applying to the Animal Health Foundation’s Boydston Fund, which helps senior citizens. Donna did and was granted $500, an amount matched by the hospital.
“I was so ecstatic, Donna said. “Are you kidding me? It’s like nothing else mattered with my Christmas. That was just pure joy. I said to Terrell: ‘Look at what we’re being given! Maybe this is an indication of a better year ahead.’”
The dental work was done on December 27. Dr. Glenn Craft, who owns Monarch, extracted Spooky’s left upper canine tooth. After the procedure, Donna said, “Dr. Craft sat with us in the lobby and talked with us. Then we talked with Dr. Alcala. They are amazing.”
Spooky, who got her name because she first showed up at the Sparacino apartment during the Halloween season in 2008, is feeling much better now. “She’s all about belly rubs. I’ll be sitting at my desk and she’ll come and start head bumping my elbow, like ‘I need attention now.’
“I feel like we’re so blessed. We have the Christmas gift of Spooky’s health. It makes us so happy. Our cats are our family.” Teddy, the new kid of the household, was adopted to be a companion to Spooky. “He’s a little rambunctious,” Donna said. “We were hoping for a little more mature male cat but we’re not giving up on him.”
How to Optomize Your Home for a Service Dog
Written By Holland Webb April 25, 2023
Article compliments of Today’s Homeowner – https://todayshomeowner.com/blog/guides/how-to-optimize-your-home-for-a-service-dog/

Why You Can Trust Us
Service dogs lead their owners into more functional and fulfilling lives. These loving, highly trained animals bear a lot of responsibility as they help perform a variety of day-to-day tasks for people with disabilities.
Most people know about guide dogs, but did you know that service dogs can also watch for signs of seizures, listen for sounds that people with hearing impairments may miss, or help open doors and carry objects for their handlers?
Service dogs are valued working partners and companions to over 500,000 Americans. Welcoming a new service dog is an exciting opportunity for you and your family.
It’s important to optimize your home for your service dog’s comfort, ease, and security. In this article, we’ll explore how to do that along with how to connect with organizations that provide service dogs and considerations for training your own service dog.
What is a Service Dog?
In addition to being great companions, working dogs perform a variety of jobs. They may aid in search-and-rescue operations, sniff out illegal substances, detect cancer, or provide therapy for people living in institutional settings.
Not every working dog is a service dog, though. The Americans with Disabilities Act specifically defines a service dog as one individually trained to do work or perform tasks for people with disabilities.
These disabilities may be physical, intellectual, psychiatric, or sensory. To qualify for a service dog, you typically need to work with an organization that serves people who live with your specific disability.
Common Service Dogs
The kind of disability you have partly determines which breed of dog you’ll get. The tiny Pomeranian, for example, lacks the physical strength to pull a wheelchair, but it has sharp hearing, a keen sense of smell, and enough dexterity to open cupboards and doors.
Labradors, Golden Retrievers, German Shepherds, and Great Danes may be employed for jobs that require physical strength and agility. Poodles are often used for tasks that require keen vision and problem-solving skills. A Pomeranian can work in tight, confined spaces due to its small size. Whatever the breed, a service dog must have qualities like intelligence, friendliness, a calm demeanor, and a love for work.
It takes about 18 months and can cost anywhere from $10,000 to $20,000 to train just one service dog. More than half of service dog candidates do not complete their training. Fortunately, these dogs can find homes as companions for loving families, while service dogs who complete their training programs go on to find work.
Optimizing Your Home for a Service Dog
When your new service dog arrives at your home, you’ll want it to feel welcome. That means optimizing your home and garden to make them accessible, navigable, and easy to work in.
Interior of the Home
Your dog needs clear, wide spaces that are simple to navigate and memorize. If you’ve had a disability for a long time, your home is probably already well-suited to your needs — and probably in good shape for your new dog, too. On the other hand, if your disability is recent, you may need to make some prompt modifications to your home.
Bathroom
The bathroom is probably the most hazardous room in your house. Every year about 235,000 people go to the emergency room because of an injury sustained in the bathroom. Small, slippery when wet, and filled with small objects in out-of-the-way cupboards, the bathroom can be tricky to manage.
Help your dog out by storing anything it needs to retrieve in a low storage container. If you use non-slip coverings on your floor, make sure they’re well-positioned to avoid either you or your dog getting tripped up.
Living Room
The clearer your floor is, the easier your dog will find it to navigate. Store remotes, magazines, throws, pillows, and other small items in baskets or bins that open from the top.
Keep personal belongings put away and debris picked up. In case of emergency, your dog will have a much easier time helping you get to safety.
You’ll also want to keep your living room well lit. If your dog will be turning lights on and off for you, be sure that switches are within easy reach of his nose or paw.
Bedroom
Most likely, your service dog will share your bedroom so it can respond to any nighttime emergencies. If your dog is a seizure detection specialist, it may need to sleep in the bed with you. If it will remain on the floor, however, make sure it has a designated sleeping spot.
You’ll also want to keep cords secured to the wall, slippers put in the closet, and pajamas picked up off the floor. Nothing should be scattered around that could distract the dog from its important job.
Kitchen
The kitchen is the primary workplace for many service dogs. Here, they may put away groceries, operate appliances, or alert their humans to alarms or smoke detectors. You’ll want to talk with your trainer about what your dog needs to do his specific jobs well.
For example, you might need to install tugs on the refrigerator doors or even remodel your kitchen so that countertops and cabinets are easy for your dog to access. Sometimes installing a lazy susan or pull-down shelf can be a great way to make your kitchen canine accessible without major renovations.
Doorways
Modern doorways are generally 32 inches wide or more to allow space for wheelchairs to get through. In an older home, however, you may be facing doors that are too small for you and your dog to pass through easily. Check with your dog’s trainer to see if your doors will be feasible for your animal to use. If not, you could have a remodeling project on your hands.
Some doorways are easy for an avid DIYer to enlarge on their own. If a door is part of a load-bearing wall, though, you need a licensed contractor to do the job.
Hallways
Narrow by nature, hallways can be a real challenge for your dog to navigate. Help your dog out by keeping them clean and clutter-free. You’ll also want to relocate furniture or decor that’s currently obscuring any part of the space.
Finally, keep this space well-lit. Maximize any natural light the space gets, and make sure overhead lights are clean and bright. If you haven’t already painted your hall a light color, now’s a good time to do that, too.
Exterior of the Home
Your dog will spend time outdoors. It’s important to keep your yard, sidewalk, and garage in good shape.
Garage and Driveway
If your dog will assist you in getting into and out of your car, it will need plenty of space to work. Trim any bushes or shrubs that extend into your driveway. You can also keep your space clear by moving other vehicles to another area outside your home. Most importantly, if your driveway is less than 12 feet wide, consider having it enlarged before your dog comes home.
Sidewalks and Pathways
Will your dog walk with you on the paths around your home or garden? If so, your sidewalk needs to be at least 36 inches wide if you use a wheelchair or 24 inches wide if you walk. Here again, you’ll want to trim any shrubs or other growth that may obscure the path or trip up your dog.
Yard
If your home has a yard, your dog needs a fence. A six-foot high barrier that discourages digging is enough for most dogs. You’ll want to check into the policies governing what kind of fence you can have in your area, and consult with the service dog trainer about the right kind of fencing for your dog’s breed and build.
General Accessibility Tips and Emergencies for Service Dogs
As you plan to welcome your service dog, look at your home as a whole space, not just a collection of individual rooms. What could you reorganize or remodel to help your dog live and work comfortably?
Avoid The Following For Your Service Dog
- Tight Spaces: Like people, dogs can’t work well in confined quarters. Find out your dog’s size, and then look for places that might feel like a tight squeeze.
- Obstructions: Your dog is probably much smaller and closer to the floor than you are. What might seem like a small obstruction to you could be a big impediment to it.
- Situations Your Dog Is Not Accustomed To: Dogs work best in predictable environments. Although service dogs are trained not to react to their surroundings, they will appreciate fewer distractions when working.
- Overstimulating Settings: While service dogs are chosen and trained to be gentle and quiet, they do experience a lot of work-related stress. Build in time for relaxation and exercise, and keep your dog out of intense environments as much as you can.
- Highly crowded Areas: Your service dog may be trained to lead you through a crowd or to provide crowd control if you have PTSD. You’ll probably want to keep your dog away from rowdy, crowded areas whenever possible, though.
Emergency Plan Tips
- Establish a safe spot for earthquakes. Make sure the area includes ample space for yourself, your dog, and any supplies both of you will need.
- Create a flood evacuation plan that your dog can follow.
- Designate an area with access to communication services during tornadoes or storms.
- Plan for power outages with an emergency kit that includes battery packs, medications, and first aid kits that the dog can reach.
Organizations that Help Find and Train Service Dogs
- The Seeing Eye
- Located in New Jersey, the Seeing Eye breeds and trains dogs to assist blind and visually impaired people. They also instruct dog owners in the proper use of handling service dogs.
- Good Fit For: People who are blind or visually impaired
- https://www.seeingeye.org/
- Assistance Dogs International
- Assistance Dogs International is a clearinghouse of programs that provide guide dogs, hearing dogs, and service dogs. The organization also accredits individual programs around the world.
- Good Fit For: Anyone looking for a service dog
- https://assistancedogsinternational.org/
- Leader Dogs for the Blind
- Fully funded by individuals and nonprofit donors, Leader Dogs for the Blind helps people who are blind or visually impaired live with independence and mobility.
- Good Fit For: People who are blind or visually impaired
- https://www.leaderdog.org/
- Epilepsy Foundation
- The Epilepsy Foundation provides resources for people interested in learning more about seizure dogs and their work. The foundation can connect you with an appropriate organization near your home.
- Good Fit For: People with epilepsy or a seizure disorder
- https://www.epilepsy.com/
- Canine Partners for Life
- Canine Partners for Life helps match people with disabilities with partner dogs. The organization provides canine partners for people with a wide variety of disabilities as well as people with diabetes and those who need a home companion.
- Good Fit For: Anyone with a qualifying disability
- https://k94life.org/
- Fidos for Freedom
- Fidos for Freedom provides trained service dogs, hearing dogs, therapy dogs, and combat-related PTSD dogs for people with disabilities, patients in health care facilities, and children with reading difficulties.
- Good Fit For: People living in the Baltimore-Washington, D.C. metropolitan community
- https://fidosforfreedom.org/
- Guide Dogs of America
- Based in Los Angeles, Guide Dogs of America breeds, raises, and trains service dogs for veterans, children with autism, and people with visual impairments. The organization also provides highly skilled dogs for jobs in hospitals, courtrooms, or classrooms.
- Good Fit For: Veterans, individuals with autism, or people with visual impairments
- https://www.guidedogsofamerica.org/
- Warrior Canine Connection
- Using a Mission Based Trauma Recovery (MBTR) model, Warrior Canine Connection helps warriors reconnect with their lives, families, friends, communities, and each other. Warriors both train and use the dogs as service partners.
- Good Fit For: Veterans, military families
- https://warriorcanineconnection.org/
- Puppies Behind Bars
- Founded in 1997, Puppies Behind Bars partners with incarcerated men and women to train service dogs and places the animals with qualifying applicants.
- Good Fit For: Veterans
- https://puppiesbehindbars.com/
- Canines for Disabled Kids
- Headquartered in Worcester, MA, Canines for Disabled Kids provides scholarships for children who need service animals. The organization also offers public education and training for families interested in acquiring a dog.
- Good Fit For: Children and families
- https://caninesforkids.org/
Tips on How to Train Your Own Service Dog
Service dogs do not have to be professionally trained. Anyone has the right to train a service dog.
However, before you begin training your own dog, make sure that he or she would make a good service dog. To be trained as a service dog the animal should meet the following criteria:
- Younger than six months old
- Spayed/neutered
- Properly sized for your needs
- Calm personality
- Long attention span
If you would like to train your own dog, consider the following best practices:
House Training
Like other house-dwelling animals, service dogs must be trained to do their business in a designated place outside. Crate-training is an effective approach since most dogs want to keep their crates clean. In the early days of training, reward the dog for going to the bathroom outside so it associates outdoor bathroom behavior with positive reinforcement.
Teaching Focus and Attentiveness Towards Handler
Your dog should focus on you — and only you — while it is working. Start this habit by encouraging the animal to make eye contact with you. Give the dog a treat for staying focused.
Off-leash Training
A service dog must respond to you whether it is on or off a leash. In a safe and controlled environment, you can take off the dog’s leash and give it simple commands. Reward or praise it for obeying those commands. Over time, you can move the activity to more-public situations.
Task-Oriented Training
Your dog is more than a companion. He or she has a job to do, and it’s up to you to train them how to do it. What do you need the animal to do?
- Be alert to seizures?
- Answer the door?
- Be alert to alarms?
- Carry groceries?
- Close doors?
- Guide you through a crowd?
- Be alert to allergens in food?
- Pull a wheelchair?
- Retrieve medication?
- Find help?
Socialization and Task-Focused Training
A successful service dog can stay focused on specific tasks even when it is out in social settings where there are distractions. Puppies should be acclimated to different sounds and people as much as possible and as early as possible. Also, be sure the dog is comfortable staying alone to minimize separation anxiety.
Disability Specific Training
Some service dogs work in disability-specific roles. For example, a hearing dog’s job is to listen for certain sounds and respond to them. A mobility assistance dog helps a human partner with limited mobility. You may want to work with a coach who can help you focus on building your dog’s unique skill set.
Emergency and Medication Focused Training
Medical alert dogs are trained to get help for those who need it. Some dogs also help manage their human’s medication. These dogs need to be individually trained to meet their job’s requirements.
Offer Relaxation Periods Between Training
Don’t forget to let your dog have fun. Off-duty time to relax, chew on a toy, get some exercise, or play with other pets is a critical part of training — and enjoying — your service dog.
Mila Gets Needed Bladder Surgery With Help from Angel Fund Grant

For more information about the Animal Health Foundation’s Angel Fund CLICK HERE
Yelena and her mother have been rescuing dogs and cats they find on the streets near their Reseda home for years, often finding them homes, if they cannot locate their owners.
That’s how they found Mila nearly two years ago. A Poddle mix, she “was running around and she was in horrible condition,” said Yelena, who asked that Pulse not use her full name. “She clearly had not been eating well and she was covered with fleas. I had to give her three baths, one after the other.
“We tried to find her owner. She did not have a chip. We posted a description of her and some people contacted us and said they thought she was their dog. But none of them sent us a picture of her and we ended up keeping her. I think we gave her a really good life.”
A few months ago, Yelena noticed that Mila “was straining to pee. I checked her and there was no blood. But I took her to the vet, who asked if I had seen any blood and if Mila was eating. The vet prescribed antibiotics, thinking the problem might be an infection.
“That seemed to help her a little bit. But then I took her to the dog park and every five seconds she was squatting down and acting like she was going to pee. And I decided I would take her either to the emergency clinic or the vet. Then I looked again and I finally saw some blood.”
Yelena called VCA McClave Animal Hospital not far from her home. “I told them exactly what was going on. They said this was an emergency, since there was blood, and to bring her in. Dr. Carina Cortez told me that they would prefer to do x-rays and a few other procedures,” Yelena said.
“I was thinking, oh this poor dog! When Dr. [Nada] Khalaf [co-medical director at McClave] called me after she saw the dog, she told me: ‘We can’t keep giving her antibiotics – we would just be going in circles.’”
Dr. Khalaf said that she saw the stone shadow on an ultrasound. She told Yelena that she suspected stones but needed radiographs to confirm they were there. When the x-rays were taken, they showed “two enormous stones in her tiny bladder,” Yelena said.
“I said that I wanted to help the dog, but I really couldn’t financially, and I asked if there was any kind of financial plan I could do. And Dr. Khalaf said she could refer me to Angel Fund. I had never heard of Angel Fund. She said: ‘I don’t know how much they can help you’ but that she would call and we would see.
“And I was thinking, ‘Oh my god, maybe they would help!’ Dr. Khalaf called back and said Angel Fund would help. I was thinking maybe $100 or $300. But the doctor said they would do more – $1,000 – and the hospital also would help, matching the grant, and that they would help me open a CareCredit account.
Dr. Cortez performed the surgery to remove the stones.
“I was really so grateful,” Yelena said. “I am just very, very thankful.” She also expressed gratitude to Dr. Khalaf: “She’s the one who helped set everything up.”
She also said that she would “rate Angel Fund at 200 on a scale of 100.” The day she learned that she was getting the grant “was a very emotional day for me.”
Mila is now doing well, she said. “After the surgery we had some antibiotics and pain medication. She was told to keep Mila from running and jumping for two weeks but the dog wanted to do just that. She now urinates normally. “She’s 100 percent different from the way she was in the dog park.
“Mila is a very special dog.”
Lessons Learned as Youth Helped Dr. Vasquez Win Prestigious Award

Dr. Vasquez and his beautiful family
By Jim Bell for SCVMA PULSE magazine 4.2023
Dr. Ronaldo (Joey) Vasquez, winner of the 2023 Cortese Lippincott Award, got lessons from his parents at an early age that would help him meet requirements for the honor.
“My parents taught me that I should give back, that we need to share,” he said in an interview. “Even if you don’t have a lot, it means a lot to people if you share. From, a young age, my parents told me that: to share, to help out.
“I remember my dad telling me, ‘Joey, if you see anyone hungry at school and they don’t have lunch, you share your lunch or buy them lunch,’” he added.
“We didn’t have a laundry machine in the house so my father and I would go to a local laundromat. And we would always see these two elderly ladies and they never had enough coins or detergent to finish their laundry. My dad always would give them quarters or share our detergent.”
The Cortese Lippincott Award is presented annually to someone who has gone “above and beyond” to make the world a better place for humans and animals, who excels in community service and education in the veterinary community and who supports the human-animal bond.
“It’s an honor to be in the same league with other winners like Jennifer Hawkins and Peter Weinstein, Dr. Vasquez said. “We got a phone call at the practice and my staff learned that I was going to get the award and they were yelling and shouting. It was one of those moments where you have to pinch yourself. Was it really happening? So I’m on cloud nine. I am just so honored to receive this award. I still think it’s unreal.”
“Veterinarians are in a unique position. Not only are they able to help pets but they also are able to positively impact humans as well. I love volunteering, giving back because it makes you feel good.”
Dr. Vasquez’ father was the late Dr. Rolando P. Vasquez, who founded North Figueroa Animal Hospital in Highland Park in 1981. His son grew up in the practice and took over as owner eight years ago when his father died.
The younger Dr. Vasquez was born in the Philippines. Shortly after his birth, his father, a practicing veterinarian, and his mother, Lucy, a veterinary technician, left him with his grandparents and immigrated to the United States.
Neither of his parents could step quickly into veterinary work in America because of licensing requirements. “They worked at various odd jobs,” Dr. Vasquez said, his mother joining the Army and working as a respiratory therapist. They sent money to the Philippines, however, to support family members. When Joey was four in 1976, there was enough money for him and his grandparents to come to California.
Young Joey had no memory of his mother and father. “When I saw them for the first time, I didn’t know they were my parents,” he said. “I was crying. I wanted to go back home.” He also met his first sibling that day, a baby girl named Patricia.
“When we opened the practice, I worked there from day one,” Dr. Vasquez recalled. “I cleaned cages, helped out with surgeries, did a lot of bathing and grooming. I did everything. I swept the parking lots, walked the dogs – I was pretty much born there.” He agrees that was part of a pretty good education for his current job of running the practice.
One problem: his dad didn’t want him to become a veterinarian. “Be like your uncle [a dentist],” he told Joey. “He works three hours a day and plays tennis the rest of the time. He makes lots of money. Veterinarians work 15 hours a day and it’s a tough job.”
After high school, Joey went to USC. “When I finished my undergrad, I really wanted to be a veterinarian. So I secretly applied to vet school. I also applied to dental school. Then I told my dad that I needed to follow my dreams and passion. And I have no regrets. This field has brought me so much happiness and it is so rewarding.”
Joey attended Ross University School of Veterinary Medicine at St. Kitts in the Caribbean, although he spent his last clinical year at the Kansas State University veterinary school.
And, yes, he now has some very long work days . But he loves every minute of it. For 10 years after he got his veterinary license in 2001, he worked full time at his father’s practice, then worked nights at an emergency hospital to widen his experience.
Despite some long hours, “working is just so enjoyable,” he said. “Putting a smile on the faces of clients is very rewarding. Sometimes all they have is their pets. And they can be so appreciative for what you have done for them.”
Dr. Vasquez said that his greatest accomplishment in life has been marrying his wife Jennifer and becoming the father of his 15-year-old son Tyler and nine-year-old daughter Kaylie. He said that he is working with his children the way his parents worked with him: encouraging them to give back and to volunteer.
“Sometimes my son goes with me to Downtown Dog Rescue and he will help out there. At Thanksgiving the whole family goes to help feed the homeless. I try to lead by example. I try to make a difference.”
Jennifer, who has an accounting background, works as office manager in the North Figueroa Hospital. She has worked there since her husband returned to the practice with his DVM degree. “I couldn’t do all I do without her,” Dr. Vasquez said.
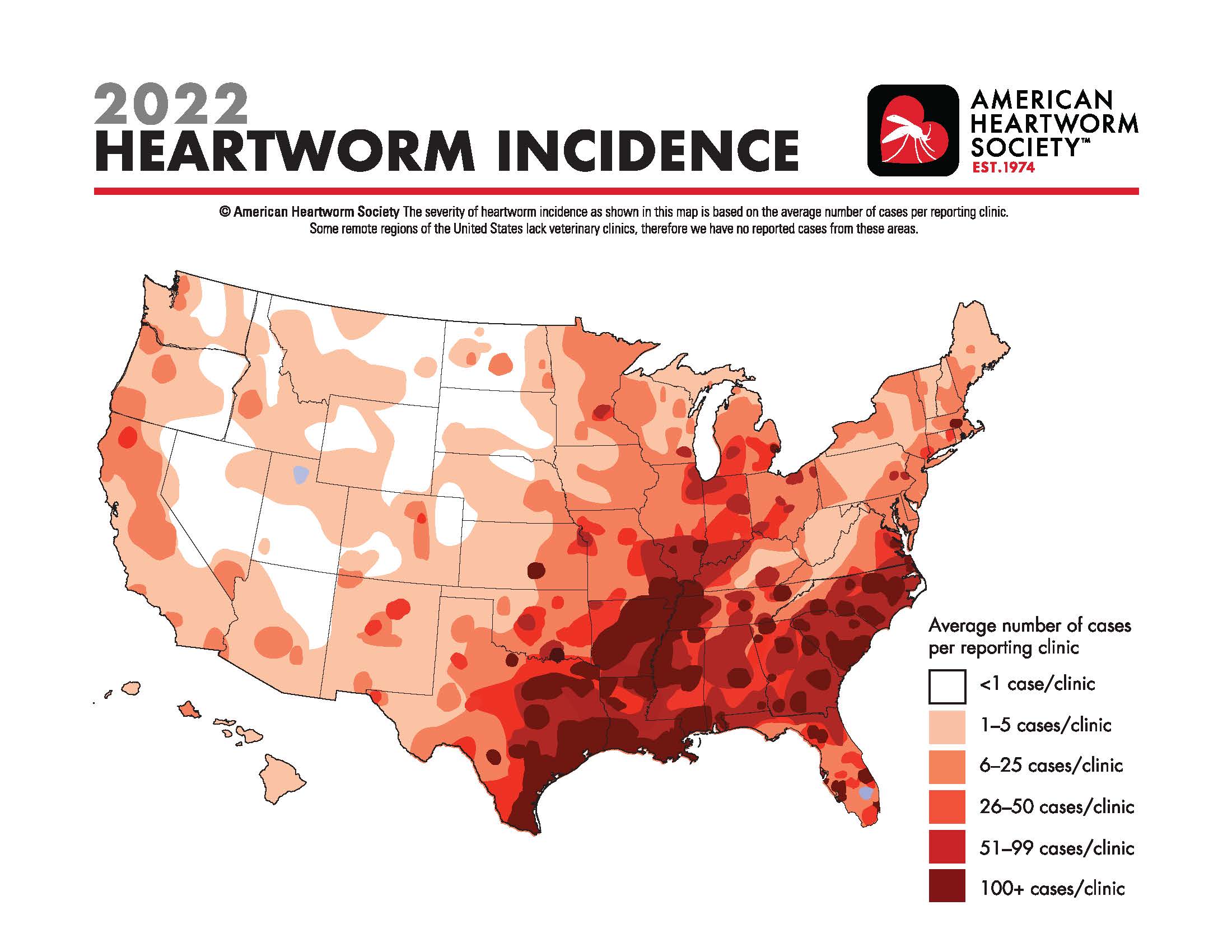
Heartworm Incidence Map
CLICK HERE TO SEE THE MAP at the American Heartworm Society
Catalyzing the field of canine comparative oncology, benefiting researchers far and wide

The Comparative Oncology Program at the National Institutes of Health is celebrating its 20th anniversary of advancing the study of cancer in dogs to help canine and human patients. AVMA News spoke with the founding and current directors of the program and two other veterinarians in the field of canine comparative oncology about their work and the importance of the program. This is the third article in a three-part series.
By Katie Burns
March 20, 2023
The Comparative Oncology Program at the National Institutes of Health has transformed canine comparative oncology since the program’s founding 20 years ago, according to Dr. Deborah W. Knapp at Purdue University and Dr. Steven Dow at Colorado State University, two of many veterinarians working in the field.
Helping pets and people
Dr. Knapp directs the Werling Comparative Oncology Research Center at Purdue University College of Veterinary Medicine and serves on the steering committee for the NIH-funded Integrated Canine Data Commons. Purdue’s program in canine comparative oncology was formed back in 1979 and has participated in the Comparative Oncology Program at the NIH since the start.

Dr. Knapp began her career working in a small animal practice, where she observed anti-cancer effects in dogs on piroxicam, a nonsteroidal anti-inflammatory drug. She studied the topic during her residency in veterinary oncology at Purdue. She later joined the Purdue veterinary faculty, and her research has focused on bladder cancer in dogs—which responds strongly to piroxicam.
Furthermore, bladder cancer in dogs is similar to muscle-invasive bladder cancer in humans. Now piroxicam is widely used in canine oncology, and there have been studies in human medicine of drugs in that class.
“I love the opportunity to help people with their pets when I know how incredibly important that is, and you form those bonds with the owners, and you’re helping their animals,” Dr. Knapp said. “And then at the same time, you’re generating information that can help human cancer patients. And for me, that’s a very special opportunity to have.”
Dr. Knapp said the Comparative Oncology Program at the NIH catalyzed the whole field—giving legitimacy to it, bringing in funding, and coordinating efforts.
Recently, Dr. Knapp and her team finished a study on early detection of bladder cancer in Scottish Terriers, with the results published by Frontiers in Oncology in November 2022. She said, “By the time we see animals with cancer, which is very similar to when physicians see people with cancer, the cancer can be pretty advanced before the diagnosis is even made.”
Scottish Terriers are at high risk of bladder cancer. The team followed 120 dogs that were at least 6 years old at the start of the study, screening them every six months for three years, and found bladder cancer in 32 of the dogs before any outward evidence of cancer. Treatment with deracoxib, another NSAID, was much more effective after finding the cancer early.
Old and new
Dr. Dow, a professor of clinical sciences at Colorado State University College of Veterinary Medicine & Biomedical Sciences, got involved with the Comparative Oncology Program at the NIH years ago when CSU was one of the sites running immunological assays in support of several studies through the program’s Comparative Oncology Trials Consortium.

Dr. Dow’s focus is developing immunotherapies for dogs with cancer. He participated in the first round of the PRE-medical Cancer Immunotherapy Network Canine Trials. The NIH funded PRECINCT first in 2017 and again at the end of 2022. Dr. Dow’s laboratory repurposes older drugs designed for other diseases, such as medications for hypertension that have immunological properties that make them promising for cancer treatment.
A recent study out of the laboratory found that using losartan, a medication for hypertension, combined with toceranib, a cancer drug, resulted in tumor stabilization or regression in half of dogs with advanced relapsed metastatic osteosarcoma to the lungs. The results of the osteosarcoma research were published in Clinical Cancer Research in February 2022.
The laboratory also studies other drug combinations that could be used in veterinary clinics now. Dr. Dow said: “These drugs, they’ve been around for a long time. They’re generic, the cost is affordable, and they have good safety margins.”
Malignant gliomas are aggressive brain tumors that share similarities between dogs and humans. A second study from Dr. Dow’s laboratory, published in Cancer Research Communications in December 2022, found that the combination of losartan and propranolol, a beta blocker, along with a cancer vaccine induced durable tumor responses in eight of 10 dogs with gliomas.
Dr. Dow said he thinks the biggest impact of the Comparative Oncology Program over the past two decades has been to increase the visibility of dogs with cancer as a translational model for humans with cancer, benefiting researchers whether or not they work directly with the program.
The role of the program has been not only creating networks, he said, “but also stimulating these interest groups that really begin to think deeply about cancer in dogs and how it applies to similar cancers in humans.”