Israeli company trains mice to sniff out contraband
Mice are effective at sniffing out explosives, drugs and other contraband, and they’re faster to train than dogs, according to Israel-based BioExplorers. The company has devised a system that directs a blast of air at a person and then into a chamber containing eight mice, who move into a second chamber when they smell contraband. WorldTribune.com
TEL AVIV — Israel has been using mice to detect explosives.
An Israeli company has developed a method that uses mice to detect hidden contraband at airports and other facilities. The company, BioExplorers, said the mice could identify anything from explosives, drugs and even cash.
 Israeli researchers claim mice are more accurate than dogs or x-ray machines at detecting explosives.
Israeli researchers claim mice are more accurate than dogs or x-ray machines at detecting explosives.
“The mice can also be easily trained, and thanks to their small size, you can use a small group of them and have multiple sensors,” BioExplorers chief technology officer Eran Lumbroso said.
The system was unveiled at the Israel Homeland Security exhibition in Tel Aviv in mid-November 2012. Executives said BioExplorers was briefing governments, police and companies on the technology.
Executives said the portable system directs a blast of air toward somebody suspected of carrying contraband. The air that strikes the person is directed into a chamber of eight mice, who sniff and move into another compartment if they detect contraband.
Lumbroso, who also founded BioExplorers, said the technology stemmed from his service in the Israel Army in 2000. At the time, the Army sought to use small animals rather than dogs to detect and foil the numerous suicide bombings by such Palestinian groups as Fatah and Hamas.
Executives said the system envisions the mice working in shifts of four hours. They said the mice can be trained much quicker than dogs.
Pet hospice increases options for pets and owners
 Veterinary at-home hospice services provide end-of-life care for ill pets, improving quality of life for animals and potentially extending life, albeit only for a few days in some cases. Hospice care must be administered by a veterinarian who works in conjunction with the pet’s regular veterinarian to provide palliative treatment such as pain management and catheter placement. San Francisco Chronicle
Veterinary at-home hospice services provide end-of-life care for ill pets, improving quality of life for animals and potentially extending life, albeit only for a few days in some cases. Hospice care must be administered by a veterinarian who works in conjunction with the pet’s regular veterinarian to provide palliative treatment such as pain management and catheter placement. San Francisco Chronicle
Shea Cox has spent her 11-year career as a veterinarian fighting to save animals’ lives.
Now, as a provider of pet hospice, she shepherds her patients through death, tending to their needs and those of their guardians, relieving animals’ pain so they can live out their final days surrounded by loved ones, not in the sterile confines of a veterinary clinic.
Modeled on human hospice, the growing field of pet hospice offers palliative care to animals in their homes. It ushers in a profound shift in how people care for dying and elderly pets, providing an option that falls between aggressive medical intervention and immediate euthanasia.
For pet owners, in-home care gives solace as they make painful end-of-life decisions.
Jeff Aoki of Oakland was in Colorado for his father’s funeral when he got a call that would only deepen his grief. His yellow Labrador, Sunny, had cancer that had spread throughout her body.
“I was devastated,” Aoki said. “Sunny was my rock, my best friend and constant companion.”
Aoki and his fiance, Sandy Wong, arranged for Sunny to receive pet hospice care from Cox. The care, which included a urinary catheter (a tumor had made it impossible for her to urinate), gave her a few extra days at home.
Aoki flew home, and for several days the couple showered Sunny with love, trips to the beach and park – and filet mignon.
When it was time to say goodbye, Cox put her to sleep in their backyard. “It was a sad, sad time but this made it so much easier,” Aoki said.
Missing plans
Cox – who was a human hospice nurse before becoming a vet – got the inspiration for her newly launched Bridge Veterinary Services while working as an ER/critical care vet at Pet Emergency Treatment and Specialty Referral Center, a Berkeley animal hospital.
“Working in that setting, I kept seeing nothing about making a plan if a patient had an incurable disease,” she said. “The choice was between either being in the hospital to get better or having to euthanize. It seemed like a disconnect; there had to be a way to offer something in between.”
With almost two-thirds of American households owning pets, it’s not surprising that attitudes toward animals’ final days have evolved from the rural past, when they were unceremoniously put down. The overwhelming majority of pet owners consider their companion animals to be family members, according to a 2011 Harris poll. At the same time, more and more people have witnessed their loved ones using human hospice.
Extending care
“We’ve decided as a culture to support human passing as compassionately as we’re able to, with hospice and palliative care,” said Oakland resident Erika Macs. As a hospital chaplain, she is intimately familiar with end-of-life issues. “It’s a natural progression that we would extend that to the animals in our lives that we’re caretakers for.”
When her 17-year-old cat, Mittens, became critically ill last year, Macs turned to Dr. Anthony Smith, a Hercules vet whose Rainbow Bridge Vet Services has offered hospice and home euthanasia for a dozen years.
“Dr. Smith was able to bring both a medical model and a sense of respectful, compassionate presence,” Macs said.
“The beauty of human hospice is it gives time to have (final) conversations,” Macs said. “With pets, it also gives time to say goodbye. The better the closure, the more quickly a person is able to heal and move on.”
Medical supervision
Pet hospice must be provided by a veterinarian because it involves medical assessments and pain medicines. Pet hospice vets coordinate with the animal’s regular vet. As in human hospice, if pets get better, they can transition back to regular medical treatment.
The costs pencil out to be more than regular check-ups but much less than invasive medical intervention. Bridge Veterinary Services, for instance, charges $250 for an initial appointment that includes a two- or three-hour at-home assessment and such initial care as inserting IV tubes or catheters.
Read more: https://www.sfgate.com/pets/article/Hospice-for-pets-comforts-owners-too-3958378.php#ixzz2FxpiHcoa
Owners and veterinarians concur: Preventive care is the best care
 Owners and veterinarians are similarly focused on preventive care, including vaccinations and parasite control, writes veterinarian Ann Hohenhaus, who discusses the results of a survey. Owners expressed concern over pet medication costs, but Dr. Hohenhaus endorses veterinary-grade medications, noting the medications are specifically designed for animals. WebMD/Tales from the Pet Clinic blog
Owners and veterinarians are similarly focused on preventive care, including vaccinations and parasite control, writes veterinarian Ann Hohenhaus, who discusses the results of a survey. Owners expressed concern over pet medication costs, but Dr. Hohenhaus endorses veterinary-grade medications, noting the medications are specifically designed for animals. WebMD/Tales from the Pet Clinic blog
By Ann Hohenhaus, DVM
Pet owners said they were primarily concerned with vaccinations, fleas and ticks, heartworms, intestinal parasites, and spending money on medications. This list appears to overlap with the veterinary list on the topic of intestinal parasites, and both owners and vets are squarely focused on preventive healthcare; care to keep their favorite furry, feathery, or scaly companion healthy.
Vaccinations
Vaccinations float to the top of most pet owners’ lists because they save pets’ lives. Before vaccinations were available for common diseases like canine distemper and feline panleukopenia, these diseases spread through neighborhoods like wildfire, often resulting in the deaths of many pets. Decreases in the recommended frequency of some vaccines, coupled with the association between injections and tumors, has raised many questions in pet owners’ minds.
Intestinal parasites
Both pet owners and veterinarians agreed intestinal parasite control was an important issue for pets. How could it not be? Intestinal parasites are high in yuck factor, high in pet discomfort, and on the list of diseases people and pets can share.
Fleas and ticks
These critters are very similar to intestinal parasites with regard to yuck factor and pet discomfort. A pet with a flea infestation may mean you also have a house or apartment with a flea infestation since fleas spend more time off your pet than on. Pet owners want to avoid an expensive exterminator bill by preventing fleas on their pet. Pet owners also want to prevent fleas and ticks to protect their pet against diseases like Lyme disease and blood parasites.
Heartworms
Because heartworms are a serious health concern in both dogs and cats, they are an important medical issue for most pet owners. Nearly every state in the United States reports cases of heartworm in resident dogs and cats. This map shows heartworm cases by state.
Year-round heartworm preventative is a “two-fer” since most prevent both heartworms and some intestinal parasites.
Pet medications
Pet owners want the best for their pet. In my mind, the best are veterinary-specific products. I prefer to prescribe medications developed specifically for veterinary patients rather than human or compounded medications. Veterinary-specific medications assure you, the pet owner, the product has been tested in dogs or cats and will be absorbed, metabolized, and effective in your pet. But, because most pets do not have insurance and medications are paid for “out of pocket,” many times pet owners can be surprised at the cost. As a pet owner myself, I believe that these veterinary-specific medications are worth paying for.
After looking carefully at the two lists of pet healthcare issues, one from pet owners and the other from veterinarians, are they really so different? Both groups’ lists really have only one item and it’s the same one: healthy, happy pets.
Funeral home offers services for 4-legged family members
 D.O. McComb & Sons’ Tribute Center in Indiana includes services for deceased pets such as burial, cremation and a private room for viewing by owners, reflecting pets’ modern status in many homes as family members.
D.O. McComb & Sons’ Tribute Center in Indiana includes services for deceased pets such as burial, cremation and a private room for viewing by owners, reflecting pets’ modern status in many homes as family members.
Memorials to pets prove it’s more than puppy love
An unusual item appeared in the newspaper the other day. It was an obituary – for a dog.
The death notice identified the dog’s owner and even included calling hours at D.O. McComb & Sons new Tribute Center on West Main Street near Lindenwood Cemetery.
While the obituary was, as far as I can recall, a first for the newspaper, the concept of special treatment for a deceased pet is nothing new.
People have been falling in love with their pets since long before Rin Tin Tin, Lassie or Old Yeller came along, sometimes with good reason. A pet will never tell you you’re ugly or overweight, and it will never ask you where you’ve been when you come home late. It will just be delighted to see you.
While your kids may prove to be crushing disappointments, a pet generally doesn’t have the wherewithal to ruin the family name, get busted for selling drugs or sell your jewelry while you’re out of town.
Truth be told, for many people, a pet is the most loyal – even the only truly loyal – creature in their lives.
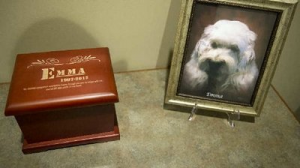
That has become evident to the people at D.O. McComb. A lot of people want a respectful exit for their pets, so when the funeral home opened the Tribute Center in October it included something unusual: a separate crematorium for pets, and a separate room, now called Emma’s Room, where a deceased pet can be briefly laid out and the owner can enter and say hello and offer one last goodbye before cremation, Dave McComb says.
It’s just a sign of the times, he said. Pets have become more important as members of the traditional family move to far-flung places. Kids leave. Wives leave. But pets remain as faithful companions and, McComb said, their status has become elevated.
Other animals, such as service dogs and police dogs, have earned a higher status in the minds of many. Maybe they don’t rate a funeral, but a thoughtful sendoff is soothing for the owners.
McComb’s can either cremate a pet and put its ashes in an urn, or arrange a burial in a portion of Riverview Cemetery that has been set aside for pets.
The funeral home hasn’t promoted the service yet, but at a Tribute Center open house, the concept drew a lot of attention and was well received, McComb said.
“We’ve had requests for even services for a while now,” McComb said.
While you won’t find preachers conducting funerals (don’t all dogs go to heaven anyway?) there can be services where an owner or friend might even eulogize an animal and friends or family members can show up and offer condolences.
“What we’ve learned is that people fall into two categories: pet owners and pet parents.”
To the pet parent, a pet becomes just as important as any other member of the family, somebody they will always remember.
The cost of a pet cremation? It varies depending on the size of the animal, which can obviously vary wildly, but the pet crematorium can handle animals up to 300 pounds.
Scientists work to crack Lyme disease’s genetic code
Researchers at The University of Texas Health Science Center at Houston are working to identify the factors that explain the virulence of Borrelia burgdorferi, the spirochete that causes Lyme disease, which affects animals and an estimated 30,000 people in the U.S. per year. Using advanced technology, the team is testing the pathogen’s 1,739 genes in an effort to find the ones responsible for its ability to spread so readily. The findings are expected to help develop vaccines, diagnostic tools and treatments
ScienceDaily (Oct. 25, 2012) — Investigators at The University of Texas Health Science Center at Houston (UTHealth) have accelerated the search for the bacterial genes that make the Lyme disease bacterium so invasive and persistent. The discovery could advance the diagnosis and treatment of this disease, which affects an estimated 30,000 Americans each year.
Scientists hope to use this information to unravel the mystery of how the spiral-shaped bacterium Borrelia burgdorferi causes Lyme disease. Ticks carry the bacterium and transfer it to animals and humans when the tiny spider-like creatures bite. The Lyme disease microorganism was discovered in 1981.
“We believe that this will be one of the most significant publications in Lyme disease in the next several years. This global approach will help ‘move the field forward’ and also serve as a model for other pathogens with similar properties,” said Steven Norris, Ph.D., the study’s senior author and the vice chair for research in the Department of Pathology and Laboratory Medicine at the UTHealth Medical School.
The bacterium can invade almost any tissue in humans or animals and trigger an infection that lasts from months to years. Its symptoms include a reddish rash that often resembles a bull’s eye and flu-like symptoms. The disease can lead to nervous system problems, joint inflammation and heart abnormalities. Most instances of Lyme disease can be treated with antibiotics.
“Our long-term goals are to screen, identify and characterize the virulence determinants of the Lyme disease bacterium and thereby dissect the mechanism of pathogenesis in mammals and ticks,” said Tao Lin, D,V.M., the study’s lead author and assistant professor of pathology and laboratory medicine at the UTHealth Medical School. “With this information, we will have a clearer picture about the virulence determinants and virulence factors for this fascinating microorganism and the mechanism of pathogenesis behind this unique, invasive, persistent pathogen.”
Norris, the Robert Greer Professor of Biomedical Sciences at UTHealth, and Lin are running tests on the 1,739 genes in the bacterium to see which genes impact the microorganism’s ability to spread disease.
To do this, they mutated the bacterial genes and gauged the impact in a mouse infection model. Overall, 4,479 mutated bacteria were isolated and characterized. Whereas it took researchers about three decades to knock out less than 40 bacterial genes, Norris and Lin knocked out 790 genes in a comparatively short period of time; some genes were “hit” multiple times. A newly developed screening technique, which involves signature-tagged mutagenesis and Luminex®-based high-throughput screening technologies, can also be used to identify infection-related genes in other bacteria.
“This kind of study enables us to better understand the disease pathogenesis at the basic level,” said Charles Ericsson, M.D., head of clinical infectious diseases at the UTHealth Medical School. “In time, such understanding of virulence properties might enable us to develop vaccine candidates, better diagnostic tools and perhaps even targeted drug intervention.”
Norris and Lin are on the faculty of The University of Texas Graduate School of Biomedical Sciences at Houston.
Previously, Norris helped develop a method based on one of the bacterium’s proteins, called VlsE, for diagnosing Lyme disease. The test, which is now used worldwide, involves detection of VlsE-specific antibodies, which are often found in people and animals infected with Lyme disease.
Also participating in the study from UTHealth were Lihui Gao, D.V.M., Chuhua Zhang, Evelyn Odeh and Loic Coutte, Ph.D. Mary B. Jacobs and Mario Philipp, Ph.D., of the Tulane University Health Sciences Center collaborated on the study as did George Chaconas, Ph.D., of The University of Calgary in Canada. Mutated strains produced through this study are being made available to the scientific community through BEI Resources.
The study is titled “Analysis of an ordered comprehensive STM mutant library in infectious Borrelia burgdorferi: insights into the genes required for mouse infectivity.” The project described was supported by Award Number R01AI059048 from the National Institute of Allergy and Infectious Diseases.
Birds can get arthritis, too
 Osteoarthritis, a painful inflammation of one or more joints, can occur in birds, but careful management by a veterinarian, along with some lifestyle changes, can help affected birds live comfortably, writes veterinarian Margaret Wissman. Diagnostic tests to ascertain the health status of the bird, including blood count, kidney and liver tests and other parameters, will help the veterinarian select the most appropriate medications, Dr. Wissman notes. Owners can make changes such as providing perches of several sizes and shapes and keeping a pet bird’s weight within the normal range to help avoid exacerbating the condition, she advises.
Osteoarthritis, a painful inflammation of one or more joints, can occur in birds, but careful management by a veterinarian, along with some lifestyle changes, can help affected birds live comfortably, writes veterinarian Margaret Wissman. Diagnostic tests to ascertain the health status of the bird, including blood count, kidney and liver tests and other parameters, will help the veterinarian select the most appropriate medications, Dr. Wissman notes. Owners can make changes such as providing perches of several sizes and shapes and keeping a pet bird’s weight within the normal range to help avoid exacerbating the condition, she advises.Arthritis is a degenerative disease of the joints that can be a primary disease or secondary to defects or injury of the joints or supporting tissues. The most common form diagnosed in pet birds is osteoarthritis. Multiple joints are often affected, unless the disease is brought on by trauma. Pain accompanies this joint inflammatory disease.
This is typically an acquired disease with age but it can be brought on by an injury or if a tumor, either malignant or non-malignant, involves a joint. Infections such as mycoplasmosis can also result in arthritis in pet birds. Affected joints may be red, swollen or hot.
You should have your bird evaluated by an avian veterinarian who will want to perform tests to ascertain the cause of the joint problems. You may want to purchase braided rope perches or soft synthetic perches, and make sure that you have perches of several different diameters so feet don’t cramp up from always being in the same position on a perch.
Have your bird’s blood count, chemistry profile, kidney and liver checked out before getting a medication prescribed. In some cases, antibiotics or antifungal medications are indicated. There are choices of NSAIDs (non-steroidal anti-inflammatories) to give a bird for long-term arthritis relief; however, most of these medications are not labeled for use in birds. The old stand-by, aspirin, is actually a wonderful anti-inflammatory for birds; however, dosing is critical, so this must be prescribed by an avian veterinarian. Other NSAIDs can also prove useful in the long-term management of arthritis. Narcotics, such as codeine, and steroids are not commonly used for long-term treatment of birds because of potentially dangerous side effects. To keep your bird more comfortable when afflicted with arthritis, provide appropriate perches as well as flat corner perches. Do not let your bird get overweight, as it will bring added stress to already damaged joints. If your bird is already overweight, discuss a long-term diet and exercise plan for your bird with your avian veterinarian.
Veterinarian makes bird nutrition his mission
 Veterinarian Joel Murphy, who runs a small-animal veterinary practice and has a passion for avian medicine, emphasizes the importance of good nutrition for pet birds. Basing his information on his study of wild birds, Dr. Murphy has developed diet recommendations for pet birds including feeding fresh vegetables and fruits, water and special pellets. According to Dr. Murphy, many pet birds in his area die prematurely due to malnutrition, a situation he believes can be prevented with owner education. He also recommends weighing birds daily because weight loss can signal illness
Veterinarian Joel Murphy, who runs a small-animal veterinary practice and has a passion for avian medicine, emphasizes the importance of good nutrition for pet birds. Basing his information on his study of wild birds, Dr. Murphy has developed diet recommendations for pet birds including feeding fresh vegetables and fruits, water and special pellets. According to Dr. Murphy, many pet birds in his area die prematurely due to malnutrition, a situation he believes can be prevented with owner education. He also recommends weighing birds daily because weight loss can signal illness
PALM HARBOR, FL — Inside the Amazon rainforest, thousands of miles from his office in Palm Harbor, the holistic veterinarian watched a colony of chattering macaws glide above the treetops.
“They looked like little blue and gold jewels filling the sky,” said Dr. Joel Murphy, recalling a research trip in 2009. “They were so beautiful, healthy and happy.”
Murphy, who taught graduate avian medicine at the University of Georgia and has lectured at veterinary schools from the Bahamas to Nepal, aims to recreate that vibrancy in the Tampa Bay area. He studies eating patterns in the wild to bring healthier diets to domestic pets.
Exotic bird owners from New Port Richey to Pinellas Park to Carrollwood seek Murphy’s unusual care, which includes blood serum tests, a self-concocted line of flower essences, and dietary counseling. But most of the sick parrots, cockatiels and parakeets Murphy encounters in the bay area — about 2,000 annually — die early from malnutrition, he said.
“It’s a huge, huge problem,” said Murphy, who runs a practice for dogs, cats and his specialty, birds, on U.S. 19 near Nebraska Avenue. “People bring me their beloved pets and have no idea what’s wrong with them.”
For years, Murphy operated an exotic bird research center in Palm Harbor. When a surprise divorce rocked his finances in 2005, he closed the operation. His continued research is independent, out of pocket.
The rainforest macaws and other exotic birds Murphy has observed nibble nuts, berries and tree bark loaded with vitamins and essential fatty acids — ingredients largely missing from many brands of pet store food.
He’s written four books and more than 100 articles related to the subject, most recently How to Care for Your Pet Bird. He constantly campaigns to visitors inside his waiting room, which he paid about $2,000 to “pet feng shui” with gold dragons and amethyst stones.
“I do everything I can to get through to people,” he said. “Proper, natural nutrition information is out there. The problem is fixable. We just need to bring attention to it.”
About eight years ago, when Clearwater resident Donna Taylor’s emerald green Amazon parrot stopped talking and eating, two emergency room referrals guided her to Murphy. She felt her pet, Billy, was close to death.
A tissue biopsy determined the bird suffered from severe liver cirrhosis. His previous owner, a restaurant manager, used to feed Billy beer, Taylor explained.
“Dr. Murphy didn’t even consider putting Billy down,” she said. “I’ve never seen that kind of compassion in a vet. Instead, we started a regimen of twice-daily holistic medications and we got five more wonderful years with him.”
Now, Taylor schedules regular appointments with Murphy to monitor the health of her Amazon, macaw and Caique birds.
“My husband and I had no idea how to correctly feed them before we talked to Dr. Murphy,” Taylor said. “Now, they only eat fresh, human-grade foods.”
To keep exotic birds healthy and happy, Murphy offers owners three basic guidelines: Provide a diet of fruits, vegetables, water and fortified pellets; weigh pets daily, because weight loss is often the first and only sign of illness in birds; and give large breeds proper training to foster good behavior (and avoid bouts of screeching and scratching).
“Birds are just like little people,” Murphy said. “You’ve got to love them and treat them as though they’re part of the family.”
8 Health benefits of having a pet
Thinking about getting a dog, cat, guinea pig, or any other kind of pet? Do it! And if you need any reason beyond the animal’s cuteness to convince someone you live with, try one of these eight health benefits that can come with pet ownership. A potentially longer, healthier life should make up for all those chewed-up shoes, pooper scoopers, and hairballs, right?
-
More physical activity:
It probably doesn’t come as a surprise that owning a dog requires a little bit of energy. Dogs have to be walked and exercised, which means dog owners are out there getting more physical activity than people without dogs. Older people are more likely to take regular walks with a dog than they are with a human, according to one study. Another found that 60% of dog owners who took their dogs for regular walks were considered to get regular moderate or vigorous exercise based on federal standards.
-
Less stress:
Sure, it can be stressful to have pets when you are afraid one might be sick or you can’t figure out how to get them to stop breaking your blinds, but overall, pets are known to reduce stress. Cortisol is a hormone activated by stress, and studies have found that being around animals can decrease cortisol levels. For this reason, many offices are starting to allow employees to bring dogs to work, and some universities are letting students borrow dogs during stressful times of the year.
-
Lower blood pressure:
Can you feel your blood pressure start to rise when stress creeps into your life? Along with medications and lifestyle changes, a pet can help with hypertension. A study of stockbrokers found that having a cat or dog helped lower the spikes in blood pressure that happen when a person is stressed. Another study of hospitalized heart patients found that dogs decreased the patients’ blood pressure by about 10% in the left side of their hearts.
-
Lower risk of heart attacks:
Good news, cat owners! Your little furball could be fighting off heart disease for you. Studies have found that people with cats were 40% less likely to have a fatal heart attack. It’s unclear whether the cat’s calming effects make the difference or whether people who choose cats as pets are less at risk for heart disease to begin with. Either way, if you’re a cat person, you’re in luck! (It’s possible that dogs have similar benefits, but the study was only done on cat owners.)
-
Alleviation of depression:
You’ve probably realized that your pets can make you smile when you’re just feeling a bit down, but even those of us suffering with diagnosed depression can reap these mood-lifting benefits. The National Institute of Mental Health recognizes animal-assisted therapy as a treatment for depression and other mood disorders because pets can have a positive effect on depression in a number of ways. A pet requires its owner to remain active and can help him or her feel less isolated from society. A pet also remains a trusted companion, even when its owner withdraws from friends and family.
-
Allergy prevention:
A seven-year study of almost 500 children found that children who were exposed to dogs and cats as babies were half as likely to have allergies and risk factors for asthma as they grew up than those who had no pets. Infants with more than one pet in the home had the lowest risk of allergies. So even though you might have to be cautious with pets around babies to make sure the pets don’t become aggressive with them, having those pets around could benefit your child in the long run.
-
Low blood sugar detection:
If you have diabetes, you know how dangerous a drop in blood sugar can be. While many people have their blood sugar under control, those who often have unexpected changes could get a life-saving health benefit from having a dog. There are specially trained dogs who have been taught to detect drops in blood sugar by smelling. When they smell a change, they can alert the person before it becomes dangerous.
-
Less risk of stroke:
This must be payment for the number of times you’ve had to clean out that disgusting litter box: owning a cat cuts a person’s risk of having a stroke by more than a third! Researchers theorize that petting a cat can lower stress or that the type of people who own cats are more stress-free naturally. Whatever the reason, you should probably go adopt a pet just to be on the safe side.
Pet trusts protect animals if they outlive their owners
 According to the 2012 AVMA pet ownership survey, there are some 164 million cats and dogs in homes across the U.S., and attorneys Elizabeth Carrie and Robert Kass recommend that pet owners plan for the possibility that they may no longer be able to care for their animals. Naming a caregiver, providing detailed pet care instructions and dedicating money specifically to the pet’s care are all important parts of the plan, according to Kass and Carrie. Bundling all the essentials into a specific, separate trust is the best way to ensure the plan will be implemented in the manner the owner intends, they said. Fox Business
According to the 2012 AVMA pet ownership survey, there are some 164 million cats and dogs in homes across the U.S., and attorneys Elizabeth Carrie and Robert Kass recommend that pet owners plan for the possibility that they may no longer be able to care for their animals. Naming a caregiver, providing detailed pet care instructions and dedicating money specifically to the pet’s care are all important parts of the plan, according to Kass and Carrie. Bundling all the essentials into a specific, separate trust is the best way to ensure the plan will be implemented in the manner the owner intends, they said. Fox Business
If you’re a parent, odds are you’ve thought about the unthinkable: Who will raise your children if something happens to you? Who do you trust to love and care for them the way you would? How do you provide the money needed and ensure that it will be used properly?
These concerns also come into play if you become disabled, even temporarily. Who can you depend on to step in until you recover?
Now consider this: there are three times as many households in the U.S. that have pets than have children- 57%, according to the American Veterinary Medicine Association’s 2012 survey .
.
Compared to the 28 million children living in this country, Americans own more than 164 million cats and dogs. Adding birds to the mix brings the total to nearly 181 million pets (not to mention horses, small animals, fish, etc.).
For many of us, our pets are our “children.” And, if you want to know they will be properly cared for in the event you can no longer do this yourself, Detroit attorneys Robert Kass and Elizabeth Carrie stress that you need to take some basic steps to ensure your wishes will be carried out.
Kass cites the case of a woman who committed suicide by jumping off a bridge. Although her body wasn’t recovered for months, it took five days for co-workers and neighbors to realize she was not just away on a trip, but actually missing. During that time her cats were without food, water, and of course, their primary human companion. “When the authorities finally went into her apartment, the cats were crazed,” he says.
If no one steps forward to take in an animal that, for whatever reason, can no longer be cared for by its owner, it is routinely taken to a shelter and put up for adoption. That’s traumatic enough. Unfortunately, unless it is a “no-kill” shelter, if it isn’t adopted within a certain period of time, an animal that was once your beloved pet, will be euthanized.
As Kass and Carrie point out in their book, Who Will Care when You’re Not There?, the biggest mistake a pet owner makes is assuming she or he will outlive her cat, dog, rabbit, African Grey. If you truly care about your pet, that’s a pretty big risk. Depending upon your age and health, the life expectancies of many species- parrots, for instance- make it very likely your pet will outlive you.
Another potential disaster is assuming that your cousin (Fast) Eddie- who always got along great with Fido on Thanksgiving visits- will: 1) know how to care for him (favorite toy, food allergies, medications, afraid of thunder, etc.) and 2) be willing to do so, even when Fido grows old and arthritic
While Eddie may, in fact, be an animal lover (he’s always been fond of the horses- the Kentucky Derby and Belmont kind), there have been sporadic family rumors about money problems. If you leave a bequest to cover the cost of Fido’s care, are you certain Eddie will use it for this purpose?
In the event Eddie surprises the family and ends up being a flawless replacement for you, what if he, himself, is incapacitated, hospitalized, or dies? Naming a successor caregiver is essential, say Kass and Carrie.
There are various avenues you can take to provide for the care of your furry and feathered “kids” if you become incapacitated. You can start with a Power of Attorney, which, unlike a typical POA (which generally covers financial assets) gives another individual the legal power to make decisions about your animal’s care. This includes everything from moving it into their own home, to giving them discretion to take it to the vet, and so forth. If the individual isn’t familiar with the pet, it’s a good idea to attach an instruction sheet listing the veterinarian and grooming names, the preferred type of food and any other important notes about the pet to help it assimilate to a new home.
However, to be on the safe side, Kass and Carrie recommend creating a free-standing trust, separate from the trust that deals with your material possessions and human children. You can fund it with an amount of money that you feel will cover the care of your pet(s) for the remainder of their lifetimes, leaving anything that remains to, perhaps, a pet-affiliated charity. They recommend using attachments to the trust since these can be easily amended as your pets and the care they need change.
Ideally, you want to have an attorney with experience in pet planning and the laws of your state draw up the documents. “If you can’t afford to do this,” says Carrie, “legalzoom.net offers pet trusts online for less than $100.” This document won’t be as customized, but it’s far better than nothing.
Consider everything you pet gives you- unconditionally and daily. Don’t you want to be sure it will receive the care it needs if and when you’re not able to provide it?
Ms. Buckner is a Retirement and Financial Planning Specialist and an instructor in Franklin Templeton Investments’ global Academy. The views expressed in this article are only those of Ms. Buckner or the individual commentator identified therein, and are not necessarily the views of Franklin Templeton Investments, which has not reviewed, and is not responsible for, the content.
Veterinarians help baby bobcat burned in forest fire
 Crews found a bobcat kitten listless and circling near the stump of a tree in the wake of fires that have burned some 73,000 acres in Northern California. Veterinarians at the Lake Tahoe Wildlife Care shelter are treating her for an eye infection and burns on all four paws. The bobcat, named Chips by her rescuers, is expected to recover and will be returned into the wild. San Francisco Chronicle/SF Gate blog (8/28)
Crews found a bobcat kitten listless and circling near the stump of a tree in the wake of fires that have burned some 73,000 acres in Northern California. Veterinarians at the Lake Tahoe Wildlife Care shelter are treating her for an eye infection and burns on all four paws. The bobcat, named Chips by her rescuers, is expected to recover and will be returned into the wild. San Francisco Chronicle/SF Gate blog (8/28)
Crews battling and cleaning up after Chips Fire, the wildfire that has blazed through almost 73,000 acres in Plumas and Lassen national forests, have come to be ready for anything — but nobody was prepared for the helpless bundle of fur they stumbled upon this weekend.
Members of the Mad River Hand Crew were patrolling and conducting mop-up operations near the north end of the fire on Saturday when they found a baby bobcat puttering along the side of the road.
Crew superintendent Tad Hair said the tiny female bobcat, which was about the size of a domestic kitten, seemed dazed and had trouble seeing. She was walking in circles near a stump, he said.
Not wanting to disrupt a wild animal from nature, the crew did a quick assessment of the kit and tried to walk away. But she began to follow the sound of their footsteps, and would curl up on Hair’s boots every time they would stop.
They brought her back to the incident command post after finding no grown bobcat tracks in the area. They contacted Lake Tahoe Wildlife Care, a nonprofit that rehabilitates injured and orphaned wildlife and returns them to the wild, and then began to care for her and prepare her for the trip to the shelter, said Laurie Pearson, a public information officer for the Chips Fire.
By then, they had taken to calling her Chips, after the fire.
Public information officer Clare Delaney said Chips was making tiny bobcat yowls as they cared for her, giving her ice chips and special kitten formula, and wiping some of the soot and ash from her fur.
“When I wiped her little face off and Laurie was holding her, she just fell right back to sleep,” she said. “[She reacted like] it was her mom licking her face.”
A firefighter transporting her to the Lake Tahoe Wildlife Care shelter flushed Chips eyes out on the way over, Pearson said. A veterinarian at the shelter found that Chips had an infection in her eyes, and after flushing them out again, and administered some ointment.
Veterinarians found that Chips also suffered second-degree burns on all four of her tiny paws, Pearson said. Until her paws are fully healed, Chips will rest on a soft bed, fattening up on six pulverized mice and more kitten formula.
Lake Tahoe Wildlife Care executive director and co-founder Cheryl Millham said she is confident Chips will regain full vision in both eyes once the infection is cleared. She said Chips is thriving and recovering nicely at the shelter.
Chips will eventually socialize with other bobcats before she is returned to the wild for good, Millham said.
Delaney said the crew became very attached to Chips.
“She was so sooty and dirty when they found her and they were worried because she was just walking in circles and was probably dehydrated,” she said. “But I think she’s got a really good start.”









