View this email in your browser What to REALLY Know About Chocolate Toxicity for Your PetThe Halloween season can be a great time to enrich your pet with walks and playtime in the falling leaves, bonding with your pet with the increased indoor time, and more. What to REALLY Know About Chocolate Toxicity for Your PetThe Halloween season can be a great time to enrich your pet with walks and playtime in the falling leaves, bonding with your pet with the increased indoor time, and more. At the same time it can be spooky for more reasons than that horror movie your partner is always trying to get you to watch! Pet owners often misunderstand the real dangers that chocolate can pose to their pet. Here are the REAL things you need to know: White chocolate poses no danger (think of a Zero bar). Milk chocolate (Hershey’s), which most Halloween candy consists of, poses a very minor risk. Dark chocolate (baker’s chocolate for example) poses a modest risk. For milk chocolate, a pet has to consume about 3 ounces of milk chocolate per 10 pounds of body weight before even a veterinarian would notice any troubling signs such as excitement (comes from theobromine in chocolate which acts like caffeine). It takes a massive amount of chocolate to be fatal. So to round out with an example, an average 20-pound dog would have to consume two full-sized candy bars (think Snicker’s bars) to even show any clinical signs. A 70-pound Labrador Retriever would have to consume 14 Butterfingers. If your dog eats a piece of chocolate, don’t worry about it, and certainly save yourself a trip to the emergency vet! The worst thing that will happen to your dog is probably digestive upset. However, if your dog is a non-stop eating machine and somehow got into a treasure trove of treats, please seek your veterinarian for treatment. I hope you all have a wonderful Halloween season and I’ll see you in November! Wags, Dr. Marty Becker Want more from Dr. Becker? Read more…Join his Facebook Group! |
Introducing Petfundr!
PetFundr provides crowdfunding for your pet’s urgent, acute or chronic care needs. With PetFundr, you can do it fast, reliably and for FREE!

Mila Gets Needed Bladder Surgery With Help from Angel Fund Grant

For more information about the Animal Health Foundation’s Angel Fund CLICK HERE
Yelena and her mother have been rescuing dogs and cats they find on the streets near their Reseda home for years, often finding them homes, if they cannot locate their owners.
That’s how they found Mila nearly two years ago. A Poddle mix, she “was running around and she was in horrible condition,” said Yelena, who asked that Pulse not use her full name. “She clearly had not been eating well and she was covered with fleas. I had to give her three baths, one after the other.
“We tried to find her owner. She did not have a chip. We posted a description of her and some people contacted us and said they thought she was their dog. But none of them sent us a picture of her and we ended up keeping her. I think we gave her a really good life.”
A few months ago, Yelena noticed that Mila “was straining to pee. I checked her and there was no blood. But I took her to the vet, who asked if I had seen any blood and if Mila was eating. The vet prescribed antibiotics, thinking the problem might be an infection.
“That seemed to help her a little bit. But then I took her to the dog park and every five seconds she was squatting down and acting like she was going to pee. And I decided I would take her either to the emergency clinic or the vet. Then I looked again and I finally saw some blood.”
Yelena called VCA McClave Animal Hospital not far from her home. “I told them exactly what was going on. They said this was an emergency, since there was blood, and to bring her in. Dr. Carina Cortez told me that they would prefer to do x-rays and a few other procedures,” Yelena said.
“I was thinking, oh this poor dog! When Dr. [Nada] Khalaf [co-medical director at McClave] called me after she saw the dog, she told me: ‘We can’t keep giving her antibiotics – we would just be going in circles.’”
Dr. Khalaf said that she saw the stone shadow on an ultrasound. She told Yelena that she suspected stones but needed radiographs to confirm they were there. When the x-rays were taken, they showed “two enormous stones in her tiny bladder,” Yelena said.
“I said that I wanted to help the dog, but I really couldn’t financially, and I asked if there was any kind of financial plan I could do. And Dr. Khalaf said she could refer me to Angel Fund. I had never heard of Angel Fund. She said: ‘I don’t know how much they can help you’ but that she would call and we would see.
“And I was thinking, ‘Oh my god, maybe they would help!’ Dr. Khalaf called back and said Angel Fund would help. I was thinking maybe $100 or $300. But the doctor said they would do more – $1,000 – and the hospital also would help, matching the grant, and that they would help me open a CareCredit account.
Dr. Cortez performed the surgery to remove the stones.
“I was really so grateful,” Yelena said. “I am just very, very thankful.” She also expressed gratitude to Dr. Khalaf: “She’s the one who helped set everything up.”
She also said that she would “rate Angel Fund at 200 on a scale of 100.” The day she learned that she was getting the grant “was a very emotional day for me.”
Mila is now doing well, she said. “After the surgery we had some antibiotics and pain medication. She was told to keep Mila from running and jumping for two weeks but the dog wanted to do just that. She now urinates normally. “She’s 100 percent different from the way she was in the dog park.
“Mila is a very special dog.”
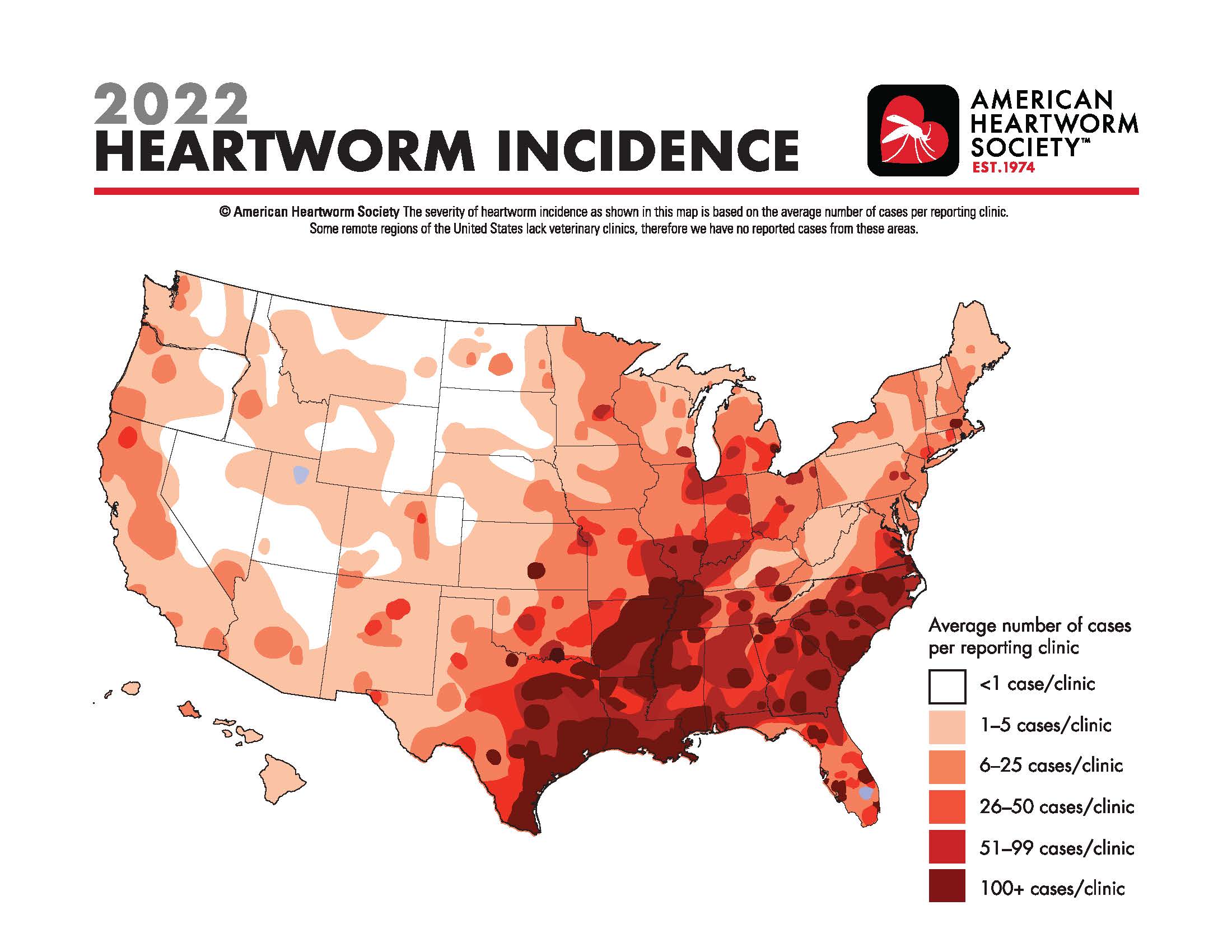
Heartworm Incidence Map
CLICK HERE TO SEE THE MAP at the American Heartworm Society
Catalyzing the field of canine comparative oncology, benefiting researchers far and wide

The Comparative Oncology Program at the National Institutes of Health is celebrating its 20th anniversary of advancing the study of cancer in dogs to help canine and human patients. AVMA News spoke with the founding and current directors of the program and two other veterinarians in the field of canine comparative oncology about their work and the importance of the program. This is the third article in a three-part series.
By Katie Burns
March 20, 2023
The Comparative Oncology Program at the National Institutes of Health has transformed canine comparative oncology since the program’s founding 20 years ago, according to Dr. Deborah W. Knapp at Purdue University and Dr. Steven Dow at Colorado State University, two of many veterinarians working in the field.
Helping pets and people
Dr. Knapp directs the Werling Comparative Oncology Research Center at Purdue University College of Veterinary Medicine and serves on the steering committee for the NIH-funded Integrated Canine Data Commons. Purdue’s program in canine comparative oncology was formed back in 1979 and has participated in the Comparative Oncology Program at the NIH since the start.

Dr. Knapp began her career working in a small animal practice, where she observed anti-cancer effects in dogs on piroxicam, a nonsteroidal anti-inflammatory drug. She studied the topic during her residency in veterinary oncology at Purdue. She later joined the Purdue veterinary faculty, and her research has focused on bladder cancer in dogs—which responds strongly to piroxicam.
Furthermore, bladder cancer in dogs is similar to muscle-invasive bladder cancer in humans. Now piroxicam is widely used in canine oncology, and there have been studies in human medicine of drugs in that class.
“I love the opportunity to help people with their pets when I know how incredibly important that is, and you form those bonds with the owners, and you’re helping their animals,” Dr. Knapp said. “And then at the same time, you’re generating information that can help human cancer patients. And for me, that’s a very special opportunity to have.”
Dr. Knapp said the Comparative Oncology Program at the NIH catalyzed the whole field—giving legitimacy to it, bringing in funding, and coordinating efforts.
Recently, Dr. Knapp and her team finished a study on early detection of bladder cancer in Scottish Terriers, with the results published by Frontiers in Oncology in November 2022. She said, “By the time we see animals with cancer, which is very similar to when physicians see people with cancer, the cancer can be pretty advanced before the diagnosis is even made.”
Scottish Terriers are at high risk of bladder cancer. The team followed 120 dogs that were at least 6 years old at the start of the study, screening them every six months for three years, and found bladder cancer in 32 of the dogs before any outward evidence of cancer. Treatment with deracoxib, another NSAID, was much more effective after finding the cancer early.
Old and new
Dr. Dow, a professor of clinical sciences at Colorado State University College of Veterinary Medicine & Biomedical Sciences, got involved with the Comparative Oncology Program at the NIH years ago when CSU was one of the sites running immunological assays in support of several studies through the program’s Comparative Oncology Trials Consortium.

Dr. Dow’s focus is developing immunotherapies for dogs with cancer. He participated in the first round of the PRE-medical Cancer Immunotherapy Network Canine Trials. The NIH funded PRECINCT first in 2017 and again at the end of 2022. Dr. Dow’s laboratory repurposes older drugs designed for other diseases, such as medications for hypertension that have immunological properties that make them promising for cancer treatment.
A recent study out of the laboratory found that using losartan, a medication for hypertension, combined with toceranib, a cancer drug, resulted in tumor stabilization or regression in half of dogs with advanced relapsed metastatic osteosarcoma to the lungs. The results of the osteosarcoma research were published in Clinical Cancer Research in February 2022.
The laboratory also studies other drug combinations that could be used in veterinary clinics now. Dr. Dow said: “These drugs, they’ve been around for a long time. They’re generic, the cost is affordable, and they have good safety margins.”
Malignant gliomas are aggressive brain tumors that share similarities between dogs and humans. A second study from Dr. Dow’s laboratory, published in Cancer Research Communications in December 2022, found that the combination of losartan and propranolol, a beta blocker, along with a cancer vaccine induced durable tumor responses in eight of 10 dogs with gliomas.
Dr. Dow said he thinks the biggest impact of the Comparative Oncology Program over the past two decades has been to increase the visibility of dogs with cancer as a translational model for humans with cancer, benefiting researchers whether or not they work directly with the program.
The role of the program has been not only creating networks, he said, “but also stimulating these interest groups that really begin to think deeply about cancer in dogs and how it applies to similar cancers in humans.”
The Troublesome Cushing’s Syndrome
March 31, 2023 / General Health / By Hemopet https://hemopet.org/the-troublesome-cushings-syndrome/?utm_source=Klaviyo&utm_medium=campaign&_kx=qjTvDeFUAmu9T1-bVDHL1OrzQOTI-Sa8jw_Kf-MGhbY%3D.Ypvfhc

Cushing’s syndrome in dogs is complex, difficult to diagnose, and tricky to treat. Before we get into all of that, we need to review the mechanisms that may cause it.
The Physiological Mechanisms
The pituitary gland is located in the brain. The adrenal glands lie near the kidneys. The pituitary gland tells the adrenal glands what to do.
How does the pituitary gland do this? Well, it releases a chemical called adrenocorticotropic hormone (ACTH). ACTH then stimulates the adrenal glands to release another hormone called cortisol, which is commonly known as the “flight or fight” stress hormone.
When the Pituitary-Adrenal Connection Goes Awry
Pituitary-Dependent (PDH) – If the pituitary gland develops a tumor that is most often benign, it will overproduce and release more ACTH. This overproduction of ACTH causes the adrenal glands to overproduce and release more cortisol. Once the pituitary gland realizes that there is an excess of cortisol circulating in the body, it will then underproduce ACTH. This form of Cushing’s disease accounts for 80-85% of the cases in dogs.
Adrenal-Dependent (ADH) – More rarely, an adrenal gland can develop a tumor that may be cancerous. This, too, can cause the release of excessive amounts of cortisol and suppresses the release of ACTH.
Drug-Related – Oral or injectable prescription glucocorticoid steroids (a class of corticosteroids) can cause another form of Cushing’s syndrome, termed “iatrogenic Cushing’s syndrome” . They suppress the adrenal glands by adding extra cortisol to help fight skin or inflammatory conditions. When given in excessive amounts or over a long period of time, they can cause the iatrogenic Cushing’s syndrome.
Atypical Cushing’s – In dogs with atypical Cushing’s syndrome due to a problem with the pituitary gland or ADH , we can observe enlargement of the liver, liver pathology, and bilaterally enlarged adrenal glands are usually present. An increased endogenous ACTH level is seen, along with the usual clinical signs, blood work results and hair coat problems. The other adrenal gland can be atrophied (shrunken). There is a decreased endogenous ACTH level and the usual clinical signs, blood work results and hair coat problems. This form of Cushing’s syndrome can be more difficult to diagnose and measurement of 17-Hyroxy (17-OHP) progesterone before and after giving ACTH is often required (see more below).
Wait! I thought it was called Cushing’s disease?
Cushing’s disease is a form of Cushing’s syndrome and specifically refers to those with PDH tumors. Cushing’s syndrome is the general state of excessive levels of cortisol in the blood. In any event, the medical term for high levels of cortisol circulating in the blood is hyperadrenocorticism.
Signs of Cushing’s Syndrome
The most telltale sign of Cushing’s syndrome is a pot-bellied appearance. Additional signs are panting, dark spots, bladder infections, thin hair and/or skin, fat pads, excessive drinking and eating, and excessive amounts of calcium deposits in the skin (calcinosis cutis/skin mineralization).
This constellation of Cushing’s signs are called Cushingoid.
Diagnosing Cushing’s Syndrome
We can analogize the current diagnostics for Cushing’s syndrome with shopping for a couch. Have you ever gone couch shopping and you like certain features from different couches, but nothing’s perfect? For instance, you like the cushions on one model, but detest the armrests? Or, you like the armrests on another, but it has an upholstered skirt that you don’t like? Let’s not even get into the length, height, depth, fabric, patterns or colors!
Anyway, Cushing’s diagnostics are similar to the variety of couches: there are a lot of options, nothing’s perfect and all of it costs a bundle. But, unlike a couch, you cannot customize the diagnostics.
This is not to negate Cushing’s testing. Indeed, you need to have positive confirmation of Cushing’s syndrome and the location of the problem (pituitary or adrenal) before medicating.
Urinary Cortisol to Creatinine Ratio (UCCR) – This test is used as a pre-screening tool to rule out Cushing’s syndrome by measuring the first morning urine at home. However, stress can cause this number to fluctuate greatly, which is why you need to collect your pet’s urine at home (one teaspoon is enough in a clean plastic dish) when he first gets up and has not exercised, and then take it into your veterinarian to run this test. Even if it is negative, and the veterinarian still highly suspects Cushing’s syndrome, further testing is necessary.
Ultrasound – An abdominal ultrasound helps by pointing us in the right direction. With PDH, both adrenal glands are abnormally enlarged. Whereas ADH, only one adrenal gland is enlarged and the other is small or atrophied.
ACTH Stimulation Test – If any dog has been given steroids in the past, this is the test experts want to use to diagnose iatrogenic Cushing’s syndrome. However, ACTH stimulation has a sensitivity of only 60%-85% (percentage of true positives), and a specificity 60%-93% (percentage of true false negatives). Additionally, it does not indicate the location causing the Cushing’s syndrome.
If this is the chosen test, it is wise to concurrently analyze 17-Hydroxyprogesterone (17-OHP) concentrations in response to ACTH administration. Dogs with atypical Cushing’s disease have an exaggerated 17-OHP response to ACTH. Other dogs with Cushing’s syndrome could have deranged steroid production pathways, such that certain steroid precursors may be abnormally increased and responsible for the presenting clinical signs, whereas cortisol concentrations are normal.
By the way, diagnosis of atypical Cushing’s disease may also include measurement of: androstenedione, estradiol, progesterone and aldosterone.
Low Dose Dexamethasone Suppression Test (LDDS) – This is considered the gold standard for testing for Cushing’s syndrome at this time unless iatrogenic Cushing’s disease is suspected. It can distinguish between PDH and ADH. The sensitivity is good at 95%, but the specificity is poor and only 50%-75%.
Endogenous ACTH (eACTH) – Endogenous ACTH should not be used to diagnose Cushing’s disease, but will help with location and secondary confirmation. The sample has to be prepared properly at the veterinarian’s office to ensure stability, then frozen, and sent frozen to a veterinary reference laboratory. Due to all of these handling factors, it is really not an ideal test unless the blood collection is at a research institution.
Zomedica has developed an in-house, point-of-care diagnostic machine that measures eACTH using bulk acoustic wave technology. (This is not an endorsement; we simply want you to know your options.) An LDDS test or ACTH will still need to be conducted.
Options to Treat Cushing’s Syndrome
If Cushing’s syndrome is confirmed, veterinarians have only a handful of treatment options. In fact, many veterinarians choose not to medicate for the disease based on bloodwork, other currently prescribed medications, additional conditions, and potential side effects of the Cushing’s disease medications.
Surgery – If it is ADH, surgical removal of the tumor is possible but can be very difficult, especially if it has spread. However, due to the complexity of removal, most cases are treated with medication.
Trilostane (Vetoryl) – At this time, this is the only prescription medication approved by the Food and Drug Administration (FDA) to treat both PDH and ADH. Trilostane works by stopping the production of cortisol in the adrenal glands. However, it should not be given to a dog that takes certain medications for heart disease, is pregnant, and/or has kidney or liver disease. Additionally, the ACTH stimulation test is preferred to monitor trilostane therapy. Return of clinical signs of Cushing’s disease can occur in some dogs while still on trilostane.
Common side effects are poor or reduced appetite, vomiting, lack of energy, diarrhea, and weakness. More serious (but considered rare) side effects include bloody diarrhea, collapse, severe sodium/potassium imbalance, and destruction of the adrenal gland that may result in death.
Selegiline (Anipryl) – Selegiline is an monoamine oxidase inhibitor (MAOI), and is also FDA approved, but only for uncomplicated PDH. It should not be given to dogs that take other MAOIs, meperidine, tramadol, tricyclic antidepressants, selective serotonin reuptake inhibitors, or alpha-2 agonists.
Side effects include vomiting, diarrhea, restlessness, disorientation/confusion, aggression, repetitive movements, tiredness, drooling, itchiness, licking, trembling, and lack of appetite. Rare, but serious side effects, include deafness and panting more than usual.
Mitotane (Lysodren) – Mitotane is a human chemotherapy drug that veterinarians can prescribe “off-label” to treat Cushing’s disease. It works by destroying the layers of the adrenal gland that produce cortisol. It should be used cautiously in pets with diabetes mellitus or kidney or liver disease. The following medications should be used with caution when given with mitotane: central nervous system (CNS) depressant drugs, fentanyl, insulin, midazolam, phenobarbital, selegiline, spironolactone, or warfarin.
Common side effects are decreased appetite, vomiting and diarrhea. Other side effects include lethargy, incoordination, weakness, or yellowing of the skin, gums, or whites of the eyes.
Regular monitoring of cortisol levels is required.
Melatonin – The enzymes that are typically elevated in HAC are inhibited by melatonin. Also, in dogs with adrenal disease treated with melatonin, repeat adrenal steroid panels show that cortisol levels are consistently reduced. Melatonin treatment for cases of mild to moderate canine adrenal disease can be effective, and particularly in cases where adrenal sex steroids are increased.
Melatonin plus phytoestrogens – Melatonin given in combination with phytoestrogens (isoflavones, lignans, and genistein) is known to inhibit adrenal steroid production. Combinations of melatonin and phytoestrogens, especially the SDG flax hull or HMR Norwegian spruce lignans have proven increased efficacy in treating these conditions.
References
“Adrenal Function Testing.” The College of Veterinary Medicine at Michigan State University, Michigan State University, https://cvm.msu.edu/vdl/laboratory-sections/endocrinology/adrenal-function-testing.
Behrend, E N et al. “Diagnosis of spontaneous canine hyperadrenocorticism: 2012 ACVIM consensus statement (small animal).” Journal of veterinary internal medicine vol. 27,6 (2013): 1292-304. doi:10.1111/jvim.12192, https://onlinelibrary.wiley.com/doi/full/10.1111/jvim.12192.
Dodds, W. Jean. “Diagnosing Atypical Cushing’s Disease/Syndrome in Dogs.” Dr. Jean Dodds’ Pet Health Resource, Tumblr, 17 Apr. 2016, https://drjeandoddspethealthresource.tumblr.com/post/142960916541/atypical-cushings-dog#.Y6CxAXbMLIW.
“Treating Cushing’s Disease in Dogs.” U.S. Food and Drug Administration, FDA, 8 July 2021, https://www.fda.gov/consumers/consumer-updates/treating-cushings-disease-dogs.
A dog died after getting bird flu in Canada. Here’s how to keep your pets safe.
See the video here: https://www.usatoday.com/story/news/health/2023/04/05/dog-dies-bird-flu-how-to-keep-pets-safe/11607516002/
Adrianna Rodriguez USA TODAY
A pet dog has died after testing positive for the highly contagious bird flu in Ontario, Canada, health officials said this week.
The Canadian Food Inspection Agency said the dog tested positive for the virus on Saturday after chewing on a wild goose. The dog subsequently developed clinical signs and died.
While further testing is underway, a necropsy showed its respiratory system may have been compromised by the virus, according to Tuesday’s statement.
Canadian health officials say it’s the first case of its kind reported in the country. The American Veterinary Medical Association says only a few cases of bird flu in cats or dogs have been reported worldwide, with none occurring in the United States.While the U.S. Department of Agriculture hasn’t reported any cases among pets, the agency has found cases in other mammals like skunks, raccoons, mountain lions, bears and foxes. Canadian health officials say it’s the first case of its kind reported in the country. The American Veterinary Medical Association says only a few cases of bird flu in cats or dogs have been reported worldwide, with none occurring in the United States.
While the U.S. Department of Agriculture hasn’t reported any cases among pets, the agency has found cases in other mammals like skunks, raccoons, mountain lions, bears and foxes.
How to keep your pet safe from bird flu
Canadian and U.S. health officials say pets’ risk of contracting and dying from bird flu appears to be very low – but not zero.
Here’s what you can do to keep your pet safe from bird flu:
►Don’t feed pets, including dogs or cats, raw meat from game birds or poultry.
►Keep pets away from dead wild birds found outside.
►Contact a veterinarian if your pet develops symptoms including fever, lethargy, lack of appetite, difficulty breathing, tremors or seizures, or conjunctivitis.
Giardiasis and Coccidiosis in Puppies
from: The Whole Dog Journal
March is Pet Poison Prevention Month
What to Do If Your Dog Eats Marijuana (Edibles, Weed, Vape Cartridges, etc.)
The amount and type of THC-containing product consumed will determine the seriousness of this event for your dog, and dictate the level of your emergency response.
By Jennifer Bailey, DVM for WHOLE DOG JOURNAL Published: January 15, 2023
Recreational marijuana has become legalized in 21 states and medical marijuana can be prescribed in 37 states. As marijuana becomes more widely available, people are looking for ways to partake of this drug without having to smoke it. This has created a market for marijuana “edibles,” also known as cannabis edibles.
Cannabis edibles are products that contain the psychoactive component of marijuana called delta-9 tetrahydrocannabinol (THC). A variety of products are available as cannabis edibles, including gummies and other candies, mints, chocolates and chocolate bars, beverages, potato chips, and baked goods such as brownies and cookies. Unfortunately, many of these sweet or savory options are also attractive to our dogs. While we may have more self-control regarding how many edibles we consume at one time, dogs are more likely to ingest an entire package of any edibles they can reach because they taste delicious.
Symptoms of THC Ingestion in Dogs
Ingestion of small to moderate amounts of THC may cause the following signs in dogs: listlessness, incoordination when walking, falling over when standing, dilated pupils, slow heart rate, dribbling urine, and an exaggerated response to light, touch, and sound. Dogs who have ingested large amounts of THC may have slow breathing, low blood pressure, and may exhibit seizures or become comatose.
What to Do If Your Dog Ate a Cannabis Product
If you observe your dog ingesting cannabis edibles, take him to your veterinarian or the closest animal emergency or urgent care facility immediately. If the ingestion occurred within 30 minutes of arrival at the hospital and your dog is not showing clinical signs of THC ingestion, then the veterinary staff may induce vomiting.
If it has been more than 30 minutes since ingestion of the edible or your dog is showing signs of listlessness, then vomiting will likely not be induced. This is because THC has an anti-emetic effect; it can suppress vomiting. If your dog is already listless, causing your dog to vomit in this depressed state can lead to aspiration pneumonia. Activated charcoal may be administered to absorb THC and minimize the effect it has on your dog’s body. If the edible contains chocolate or xylitol, then additional treatments may be necessary.
What If You Are Not Sure If Your Dog Ate a Cannabis Product?
If your dog is exhibiting signs of THC ingestion, but you did not witness or find evidence of this, have your dog evaluated by a veterinarian immediately. Be honest about what you have in the home, including any products containing THC, prescription sedatives, vape cartridges (including nicotine), and illicit drugs. Children, seniors, and roommates living in the home may not always be forthcoming about what they are storing in their bedrooms, so be firm yet gentle when inquiring about the presence of these products. The veterinary staff wants only to help your dog. They are not interested in contacting authorities about anything illegal in your home.
The clinical signs of THC ingestion look similar to the signs associated with ingestion of other sedatives, nicotine, and antifreeze. There is an antidote for antifreeze ingestion and without this intervention, this toxicity is always fatal. Your veterinarian may want to complete additional testing to rule out other causes for your dog’s clinical signs so that the appropriate treatment plan is initiated.
Although there is a urine test for THC available for use in people, this test is not always accurate in dogs. Dogs metabolize THC differently than people, so there is a high rate of false negatives with this test. However, a positive test for THC is almost always compatible with THC ingestion.
If ingestion of THC is suspected and the potential source has been identified, the veterinary team may contact animal poison control for further guidance regarding treatment. There are a number of variables that can alter how THC affects your dog. These variables include how much was ingested, your dog’s weight and concurrent medical conditions, any medications or supplements your dog may be taking, how the THC was infused into the product, and if the edible contains chocolate or xylitol.
Brownies, chocolates, and chocolate bars containing THC add another dimension to your dog’s toxicity: ingestion of theobromine and caffeine. Both of these are contained in chocolate and are toxic to your dog. Just like with THC, the type of chocolate (such as dark or milk chocolate), the amount ingested and the weight of your dog dictate the danger level and recommended treatment. (See “What to Do If Your Dog Eats Chocolate.”)
Gummies, mints, other THC edible candies and even baked goods may contain xylitol, an artificial sweetener that is toxic to dogs. Even tiny doses of xylitol are toxic to dogs, so it is important to know if any edibles your dog may have consumed contain xylitol.
Treatment for Cannabis Ingestion
Most mild cases of THC ingestion can be treated successfully at home by keeping your dog in a safe, quiet room where he cannot fall down the stairs or be exposed to excessive light or sound. Moderate cases of THC ingestion may require hospitalization with intravenous fluids, monitoring of heart rate and blood pressure, and medications to support the cardiovascular system and treat neurologic signs. Ingestion of high doses of THC will require hospitalization and may necessitate the administration of intralipids. Intralipids bind to THC so that it can be excreted safely from the body.
Ingested THC is fat soluble and is readily stored in body fat. Therefore, it can take anywhere from 12 to 36 hours for your dog’s clinical signs to resolve after ingesting a cannabis edible.
If you use cannabis products, store them in a locked drawer or cabinet. Dogs are clever and some can open drawers and cabinets, but I have yet to meet one that can insert a key in a lock!
Dr. Jennifer Bailey is a 2012 graduate of the Western University of Health Sciences College of Veterinary Medicine. She is an emergency and urgent care veterinarian at an emergency and specialty practice in Syracuse, New York.
How do dogs get parvo? Here’s how to spot symptoms, what to know on spread of pet disease.
USA TODAY https://www.usatoday.com/story/news/2022/12/08/how-do-dogs-get-parvo/10702650002/
The spread of disease — person to person, through a sneeze or a loud exclamation, or via an unwashed surface — has been a hot topic of conversation in recent years. Plenty of people now know a great deal about how to slow the spread of illness. Do those same rules apply when it comes to the animal world?
Parvo, for example, is a common virus among dogs. How can canines stay protected? Get vaccinated and stay vigilant, just like us. Here’s what you need to know about the disease that affects puppies of all kinds:
How is parvo spread in dogs?
Dogs contract the highly contagious virus through dog-to-dog interaction or contact with an infected surface, environment, or person, the American Veterinary Medical association reports.
What is parvo?:Understand parvo in dogs with this definitive guide to the illness.
Despite there being an effective vaccine for the illness, parvo remains fairly common, Dr. Whitney Miller, Petco’s chief veterinarian told USA TODAY. This is in part because it is able to withstand weather conditions and live in the environment for upwards of 6 months to a year, Dr. Miller reports.
Pet Care 101:What to know about your pet’s health and common behaviors
What foods are safe for dogs to eat? Here’s what human foods are and are not safe for your pet.
What are parvo symptoms?
“Parvo is a viral disease that attacks a dog’s immune and GI systems,” Dr. Miller says, so the first sign a dog owner might see is their pet losing a healthy appetite.
This might eventually progress to “potentially bloody diarrhea and vomiting” she reports. This can dehydrate your dog, making it imperative to seek treatment sooner rather than later.
The American Kennel Club lists potential symptoms as:
- Bloody diarrhea
- Vomiting
- Fever
- Lethargy
- Loss of appetite
- Weight loss
- Weakness
- Dehydration
- Depression
Is parvo contagious to other dogs?
Parvo is highly contagious, so if your dog has been in contact with a known infected pet or environment it is wise to seek treatment sooner rather than later.
There is an effective vaccine against the disease, and it is much more common for young dogs or unvaccinated canines to contract the disease. “The number one recommendation is to make sure that when your dog’s a puppy that they start on their vaccination schedule,” Miller says.
How likely is a puppy to get parvo?
This depends on a number of factors: how common parvo is in the environment where you live, how your puppy is, if they are vaccinated, and how social they are.
Since parvo can be spread through dog-to-dog contact, if your dog is highly social, often visiting dog parks or staying at a doggy day-care, they may be at a higher risk.
Dogs between 6 weeks old and 6 months are also at a higher risk, along with unvaccinated puppies, the American Kennel Club reports.
Certain dog breeds are also more susceptible to parvo AKC reports, including:
- Rottweilers Doberman Pinschers
- American Staffordshire Terriers
- English Springer Spaniels
- German Shepherd Dogs
- Labrador Retrievers
How many parvo shots does a dog need?
Three. The American Kennel Club reports that vaccination against parvo is a 3 shot series, and that owners should be particularly careful during the time in between shots so that their pup does not contract the illness.
Dogs should receive this shot series as puppies, when they are most vulnerable, ideally between starting at the age of 6 weeks.
How much does it cost to treat parvo?
There is no definitive cost that can be put on treating parvo.
Treatment depends on the severity of the illness, and in severe cases could involve a trip to emergency care which can be quite pricey. In less severe cases, the course of treatment is supportive care — rehydration efforts and keeping your dog warm as they recover.
The total cost of such care depends on those variety of factors, including pet insurance and the seriousness of the condition.
More Stories
AOC under investigation: House Ethics Committee probes Ocasio-CortezNEWS
Republican Herschel Walker speaks after defeat in Georgia Senate raceNEWS
UNICEF Is Fighting Against the Global Food CrisisUNICEF USA|
© 2022 USA TODAY, a division of Gannett Satellite Information Network, LLC.
javascript:void(0)about:blank
about:blankabout:blank

about:blankabout:blankabout:blankabout:blankabout:blank

