Swim Safety for Dogs
Contrary to popular belief, not all dogs automatically know how to swim. Here’s how to teach a dog to swim – and how to improve the water safety of dogs who already swim well.
Published:March 4, 2023Updated:March 3, 2023

The term “dog paddle” has become synonymous with staying afloat in the water. It’s the first swim stroke most children learn – moving their hands and legs alternately – in a way that’s similar to how experienced dogs and other quadrupedal mammals swim.
The key word is “experienced.” Inexperienced (or panicked) dogs often concentrate their efforts on the front legs, forgetting to fire up the back end. Front-end-only swimming is ineffective and leaves dogs near-vertical in the water. It creates a lot of disorienting splashing, requires tremendous energy, and is a dangerous way for your dog to enjoy a dip in the pool, lake, or ocean.
The following two tips will help your dog improve his swim stroke:
- Support your dog’s back end. Joining your dog in the water and gently supporting his back end as he swims can help him learn to level out and begin using his front and rear legs in unison. For dogs who still lag in kicking their rear legs, touching their feet underwater can prompt kicking.
- Use a well-fitted life jacket. A dog life jacket can help keep your dog afloat and help anxious swimmers begin to relax enough to think about paddling with all four legs. (See “Dog Life Jacket Review,” WDJ August 2021, for recommendations.)
Safety for swimmers
Keep these things in mind to help ensure safe swimming:
- Body type matters! Your dog’s breed, build, and overall health have a lot to do with how effectively she can handle herself in the water. Breeds with broad chests and shorter legs (Bulldogs, Corgis, Pugs, etc.) aren’t designed for effective swimming. Heavily muscled dogs – like many of the so-called “bully” breeds – exert a lot of energy in the water due to their greater body mass.
- Teach your dog to safely enter and exit the pool. Ideally, your dog will enter and exit the pool only via the steps. Even accomplished swimmers can drown while unsuccessfully trying to claw their way out from the edge of the pool. And dog cannonball entrances, while fun to watch, are unsafe when dogs and people are simultaneously in the water.
Start by making the top step of the pool a great place to be by feeding your dog high-value treats at that location. Eventually carry or guide your dog into the water a few feet from the steps and release him to swim back to the steps where a party awaits. Repeat until your dog is patterned to head toward the steps from any direction.
- Everything in moderation. Swimming is a great way for dogs to burn excess energy, stay in shape, and even shed some unwanted pounds, but don’t overdo it. The more overweight the dog, the faster he will tire. Watch out for “weekend warrior syndrome,” where a dog who is mostly sedentary suddenly gets too much exercise. Dogs, like people, experience muscle soreness and stiffness.
Swim school for dogs
If you want to make sure your dog will be safe near and in the water, but aren’t comfortable teaching the skills yourself, look for a positive reinforcement trainer to help you. Many dog trainers offer water safety training and many training facilities features pools where your dog can perfect his skills and enjoy fun water play.
Introducing Petfundr!
PetFundr provides crowdfunding for your pet’s urgent, acute or chronic care needs. With PetFundr, you can do it fast, reliably and for FREE!

Boydston Senior Grant Helps Lulu Find New Lease on Her Life

Noreen Sturges, who lost her 15-year-old canine companion Papillon last year, found a replacement a few months ago in Lulu, a female Maltese. “Lulu was rather matted, had a hacking cough and needed care and lots of love,” Noreen said.
Lulu had belonged to a family that was no longer able to provide her with the care and attention she needed. When Lulu was brought to Noreen’s home, “it was love at first sight,” she said.
Noreen hired a groomer to attend to Lulu’s matted hair. After the grooming, Noreen took Lulu to Monarch Veterinary Hospital in Laguna Niguel not far from her home.
Dr. Kelly Alcala examined her and found some serious dental issues that would require surgery and the extraction of some teeth. Lulu also had a hacking cough – “not like she would have had with a cold,” Noreen said. Dr. Alcala told her that she thought decay from the dog’s teeth was getting into her digestive system and probably causing the cough, Noreen said.
The doctor suggested that Noreen apply for a Boydston Grant to help pay for Lulu’s treatment and surgery. A grant of $500 was approved and Dr. Alacala did the surgery. The dog is now thriving, Noreen said, and the hacking cough is gone.
Lulu is eating her new diet voraciously. “And she’s a love!” Noreen said. “Everything’s good now.” The dog, she said, “is running around – up and down the stairs and all over the place.
“I didn’t think I could ever love a dog as much as my Papillon, “but I just love Lulu.”
She added that she is grateful for the help provided by her Boydston grant and the matching sum from Monarch Hospital, as well as for the work of Dr. Alcala. “I just love her, too,” she said.
Noreen said that she and Lulu “are having a lovely time together. She is quite a companion.”
How to Optomize Your Home for a Service Dog
Written By Holland Webb April 25, 2023
Article compliments of Today’s Homeowner – https://todayshomeowner.com/blog/guides/how-to-optimize-your-home-for-a-service-dog/

Why You Can Trust Us
Service dogs lead their owners into more functional and fulfilling lives. These loving, highly trained animals bear a lot of responsibility as they help perform a variety of day-to-day tasks for people with disabilities.
Most people know about guide dogs, but did you know that service dogs can also watch for signs of seizures, listen for sounds that people with hearing impairments may miss, or help open doors and carry objects for their handlers?
Service dogs are valued working partners and companions to over 500,000 Americans. Welcoming a new service dog is an exciting opportunity for you and your family.
It’s important to optimize your home for your service dog’s comfort, ease, and security. In this article, we’ll explore how to do that along with how to connect with organizations that provide service dogs and considerations for training your own service dog.
What is a Service Dog?
In addition to being great companions, working dogs perform a variety of jobs. They may aid in search-and-rescue operations, sniff out illegal substances, detect cancer, or provide therapy for people living in institutional settings.
Not every working dog is a service dog, though. The Americans with Disabilities Act specifically defines a service dog as one individually trained to do work or perform tasks for people with disabilities.
These disabilities may be physical, intellectual, psychiatric, or sensory. To qualify for a service dog, you typically need to work with an organization that serves people who live with your specific disability.
Common Service Dogs
The kind of disability you have partly determines which breed of dog you’ll get. The tiny Pomeranian, for example, lacks the physical strength to pull a wheelchair, but it has sharp hearing, a keen sense of smell, and enough dexterity to open cupboards and doors.
Labradors, Golden Retrievers, German Shepherds, and Great Danes may be employed for jobs that require physical strength and agility. Poodles are often used for tasks that require keen vision and problem-solving skills. A Pomeranian can work in tight, confined spaces due to its small size. Whatever the breed, a service dog must have qualities like intelligence, friendliness, a calm demeanor, and a love for work.
It takes about 18 months and can cost anywhere from $10,000 to $20,000 to train just one service dog. More than half of service dog candidates do not complete their training. Fortunately, these dogs can find homes as companions for loving families, while service dogs who complete their training programs go on to find work.
Optimizing Your Home for a Service Dog
When your new service dog arrives at your home, you’ll want it to feel welcome. That means optimizing your home and garden to make them accessible, navigable, and easy to work in.
Interior of the Home
Your dog needs clear, wide spaces that are simple to navigate and memorize. If you’ve had a disability for a long time, your home is probably already well-suited to your needs — and probably in good shape for your new dog, too. On the other hand, if your disability is recent, you may need to make some prompt modifications to your home.
Bathroom
The bathroom is probably the most hazardous room in your house. Every year about 235,000 people go to the emergency room because of an injury sustained in the bathroom. Small, slippery when wet, and filled with small objects in out-of-the-way cupboards, the bathroom can be tricky to manage.
Help your dog out by storing anything it needs to retrieve in a low storage container. If you use non-slip coverings on your floor, make sure they’re well-positioned to avoid either you or your dog getting tripped up.
Living Room
The clearer your floor is, the easier your dog will find it to navigate. Store remotes, magazines, throws, pillows, and other small items in baskets or bins that open from the top.
Keep personal belongings put away and debris picked up. In case of emergency, your dog will have a much easier time helping you get to safety.
You’ll also want to keep your living room well lit. If your dog will be turning lights on and off for you, be sure that switches are within easy reach of his nose or paw.
Bedroom
Most likely, your service dog will share your bedroom so it can respond to any nighttime emergencies. If your dog is a seizure detection specialist, it may need to sleep in the bed with you. If it will remain on the floor, however, make sure it has a designated sleeping spot.
You’ll also want to keep cords secured to the wall, slippers put in the closet, and pajamas picked up off the floor. Nothing should be scattered around that could distract the dog from its important job.
Kitchen
The kitchen is the primary workplace for many service dogs. Here, they may put away groceries, operate appliances, or alert their humans to alarms or smoke detectors. You’ll want to talk with your trainer about what your dog needs to do his specific jobs well.
For example, you might need to install tugs on the refrigerator doors or even remodel your kitchen so that countertops and cabinets are easy for your dog to access. Sometimes installing a lazy susan or pull-down shelf can be a great way to make your kitchen canine accessible without major renovations.
Doorways
Modern doorways are generally 32 inches wide or more to allow space for wheelchairs to get through. In an older home, however, you may be facing doors that are too small for you and your dog to pass through easily. Check with your dog’s trainer to see if your doors will be feasible for your animal to use. If not, you could have a remodeling project on your hands.
Some doorways are easy for an avid DIYer to enlarge on their own. If a door is part of a load-bearing wall, though, you need a licensed contractor to do the job.
Hallways
Narrow by nature, hallways can be a real challenge for your dog to navigate. Help your dog out by keeping them clean and clutter-free. You’ll also want to relocate furniture or decor that’s currently obscuring any part of the space.
Finally, keep this space well-lit. Maximize any natural light the space gets, and make sure overhead lights are clean and bright. If you haven’t already painted your hall a light color, now’s a good time to do that, too.
Exterior of the Home
Your dog will spend time outdoors. It’s important to keep your yard, sidewalk, and garage in good shape.
Garage and Driveway
If your dog will assist you in getting into and out of your car, it will need plenty of space to work. Trim any bushes or shrubs that extend into your driveway. You can also keep your space clear by moving other vehicles to another area outside your home. Most importantly, if your driveway is less than 12 feet wide, consider having it enlarged before your dog comes home.
Sidewalks and Pathways
Will your dog walk with you on the paths around your home or garden? If so, your sidewalk needs to be at least 36 inches wide if you use a wheelchair or 24 inches wide if you walk. Here again, you’ll want to trim any shrubs or other growth that may obscure the path or trip up your dog.
Yard
If your home has a yard, your dog needs a fence. A six-foot high barrier that discourages digging is enough for most dogs. You’ll want to check into the policies governing what kind of fence you can have in your area, and consult with the service dog trainer about the right kind of fencing for your dog’s breed and build.
General Accessibility Tips and Emergencies for Service Dogs
As you plan to welcome your service dog, look at your home as a whole space, not just a collection of individual rooms. What could you reorganize or remodel to help your dog live and work comfortably?
Avoid The Following For Your Service Dog
- Tight Spaces: Like people, dogs can’t work well in confined quarters. Find out your dog’s size, and then look for places that might feel like a tight squeeze.
- Obstructions: Your dog is probably much smaller and closer to the floor than you are. What might seem like a small obstruction to you could be a big impediment to it.
- Situations Your Dog Is Not Accustomed To: Dogs work best in predictable environments. Although service dogs are trained not to react to their surroundings, they will appreciate fewer distractions when working.
- Overstimulating Settings: While service dogs are chosen and trained to be gentle and quiet, they do experience a lot of work-related stress. Build in time for relaxation and exercise, and keep your dog out of intense environments as much as you can.
- Highly crowded Areas: Your service dog may be trained to lead you through a crowd or to provide crowd control if you have PTSD. You’ll probably want to keep your dog away from rowdy, crowded areas whenever possible, though.
Emergency Plan Tips
- Establish a safe spot for earthquakes. Make sure the area includes ample space for yourself, your dog, and any supplies both of you will need.
- Create a flood evacuation plan that your dog can follow.
- Designate an area with access to communication services during tornadoes or storms.
- Plan for power outages with an emergency kit that includes battery packs, medications, and first aid kits that the dog can reach.
Organizations that Help Find and Train Service Dogs
- The Seeing Eye
- Located in New Jersey, the Seeing Eye breeds and trains dogs to assist blind and visually impaired people. They also instruct dog owners in the proper use of handling service dogs.
- Good Fit For: People who are blind or visually impaired
- https://www.seeingeye.org/
- Assistance Dogs International
- Assistance Dogs International is a clearinghouse of programs that provide guide dogs, hearing dogs, and service dogs. The organization also accredits individual programs around the world.
- Good Fit For: Anyone looking for a service dog
- https://assistancedogsinternational.org/
- Leader Dogs for the Blind
- Fully funded by individuals and nonprofit donors, Leader Dogs for the Blind helps people who are blind or visually impaired live with independence and mobility.
- Good Fit For: People who are blind or visually impaired
- https://www.leaderdog.org/
- Epilepsy Foundation
- The Epilepsy Foundation provides resources for people interested in learning more about seizure dogs and their work. The foundation can connect you with an appropriate organization near your home.
- Good Fit For: People with epilepsy or a seizure disorder
- https://www.epilepsy.com/
- Canine Partners for Life
- Canine Partners for Life helps match people with disabilities with partner dogs. The organization provides canine partners for people with a wide variety of disabilities as well as people with diabetes and those who need a home companion.
- Good Fit For: Anyone with a qualifying disability
- https://k94life.org/
- Fidos for Freedom
- Fidos for Freedom provides trained service dogs, hearing dogs, therapy dogs, and combat-related PTSD dogs for people with disabilities, patients in health care facilities, and children with reading difficulties.
- Good Fit For: People living in the Baltimore-Washington, D.C. metropolitan community
- https://fidosforfreedom.org/
- Guide Dogs of America
- Based in Los Angeles, Guide Dogs of America breeds, raises, and trains service dogs for veterans, children with autism, and people with visual impairments. The organization also provides highly skilled dogs for jobs in hospitals, courtrooms, or classrooms.
- Good Fit For: Veterans, individuals with autism, or people with visual impairments
- https://www.guidedogsofamerica.org/
- Warrior Canine Connection
- Using a Mission Based Trauma Recovery (MBTR) model, Warrior Canine Connection helps warriors reconnect with their lives, families, friends, communities, and each other. Warriors both train and use the dogs as service partners.
- Good Fit For: Veterans, military families
- https://warriorcanineconnection.org/
- Puppies Behind Bars
- Founded in 1997, Puppies Behind Bars partners with incarcerated men and women to train service dogs and places the animals with qualifying applicants.
- Good Fit For: Veterans
- https://puppiesbehindbars.com/
- Canines for Disabled Kids
- Headquartered in Worcester, MA, Canines for Disabled Kids provides scholarships for children who need service animals. The organization also offers public education and training for families interested in acquiring a dog.
- Good Fit For: Children and families
- https://caninesforkids.org/
Tips on How to Train Your Own Service Dog
Service dogs do not have to be professionally trained. Anyone has the right to train a service dog.
However, before you begin training your own dog, make sure that he or she would make a good service dog. To be trained as a service dog the animal should meet the following criteria:
- Younger than six months old
- Spayed/neutered
- Properly sized for your needs
- Calm personality
- Long attention span
If you would like to train your own dog, consider the following best practices:
House Training
Like other house-dwelling animals, service dogs must be trained to do their business in a designated place outside. Crate-training is an effective approach since most dogs want to keep their crates clean. In the early days of training, reward the dog for going to the bathroom outside so it associates outdoor bathroom behavior with positive reinforcement.
Teaching Focus and Attentiveness Towards Handler
Your dog should focus on you — and only you — while it is working. Start this habit by encouraging the animal to make eye contact with you. Give the dog a treat for staying focused.
Off-leash Training
A service dog must respond to you whether it is on or off a leash. In a safe and controlled environment, you can take off the dog’s leash and give it simple commands. Reward or praise it for obeying those commands. Over time, you can move the activity to more-public situations.
Task-Oriented Training
Your dog is more than a companion. He or she has a job to do, and it’s up to you to train them how to do it. What do you need the animal to do?
- Be alert to seizures?
- Answer the door?
- Be alert to alarms?
- Carry groceries?
- Close doors?
- Guide you through a crowd?
- Be alert to allergens in food?
- Pull a wheelchair?
- Retrieve medication?
- Find help?
Socialization and Task-Focused Training
A successful service dog can stay focused on specific tasks even when it is out in social settings where there are distractions. Puppies should be acclimated to different sounds and people as much as possible and as early as possible. Also, be sure the dog is comfortable staying alone to minimize separation anxiety.
Disability Specific Training
Some service dogs work in disability-specific roles. For example, a hearing dog’s job is to listen for certain sounds and respond to them. A mobility assistance dog helps a human partner with limited mobility. You may want to work with a coach who can help you focus on building your dog’s unique skill set.
Emergency and Medication Focused Training
Medical alert dogs are trained to get help for those who need it. Some dogs also help manage their human’s medication. These dogs need to be individually trained to meet their job’s requirements.
Offer Relaxation Periods Between Training
Don’t forget to let your dog have fun. Off-duty time to relax, chew on a toy, get some exercise, or play with other pets is a critical part of training — and enjoying — your service dog.
Mila Gets Needed Bladder Surgery With Help from Angel Fund Grant

For more information about the Animal Health Foundation’s Angel Fund CLICK HERE
Yelena and her mother have been rescuing dogs and cats they find on the streets near their Reseda home for years, often finding them homes, if they cannot locate their owners.
That’s how they found Mila nearly two years ago. A Poddle mix, she “was running around and she was in horrible condition,” said Yelena, who asked that Pulse not use her full name. “She clearly had not been eating well and she was covered with fleas. I had to give her three baths, one after the other.
“We tried to find her owner. She did not have a chip. We posted a description of her and some people contacted us and said they thought she was their dog. But none of them sent us a picture of her and we ended up keeping her. I think we gave her a really good life.”
A few months ago, Yelena noticed that Mila “was straining to pee. I checked her and there was no blood. But I took her to the vet, who asked if I had seen any blood and if Mila was eating. The vet prescribed antibiotics, thinking the problem might be an infection.
“That seemed to help her a little bit. But then I took her to the dog park and every five seconds she was squatting down and acting like she was going to pee. And I decided I would take her either to the emergency clinic or the vet. Then I looked again and I finally saw some blood.”
Yelena called VCA McClave Animal Hospital not far from her home. “I told them exactly what was going on. They said this was an emergency, since there was blood, and to bring her in. Dr. Carina Cortez told me that they would prefer to do x-rays and a few other procedures,” Yelena said.
“I was thinking, oh this poor dog! When Dr. [Nada] Khalaf [co-medical director at McClave] called me after she saw the dog, she told me: ‘We can’t keep giving her antibiotics – we would just be going in circles.’”
Dr. Khalaf said that she saw the stone shadow on an ultrasound. She told Yelena that she suspected stones but needed radiographs to confirm they were there. When the x-rays were taken, they showed “two enormous stones in her tiny bladder,” Yelena said.
“I said that I wanted to help the dog, but I really couldn’t financially, and I asked if there was any kind of financial plan I could do. And Dr. Khalaf said she could refer me to Angel Fund. I had never heard of Angel Fund. She said: ‘I don’t know how much they can help you’ but that she would call and we would see.
“And I was thinking, ‘Oh my god, maybe they would help!’ Dr. Khalaf called back and said Angel Fund would help. I was thinking maybe $100 or $300. But the doctor said they would do more – $1,000 – and the hospital also would help, matching the grant, and that they would help me open a CareCredit account.
Dr. Cortez performed the surgery to remove the stones.
“I was really so grateful,” Yelena said. “I am just very, very thankful.” She also expressed gratitude to Dr. Khalaf: “She’s the one who helped set everything up.”
She also said that she would “rate Angel Fund at 200 on a scale of 100.” The day she learned that she was getting the grant “was a very emotional day for me.”
Mila is now doing well, she said. “After the surgery we had some antibiotics and pain medication. She was told to keep Mila from running and jumping for two weeks but the dog wanted to do just that. She now urinates normally. “She’s 100 percent different from the way she was in the dog park.
“Mila is a very special dog.”
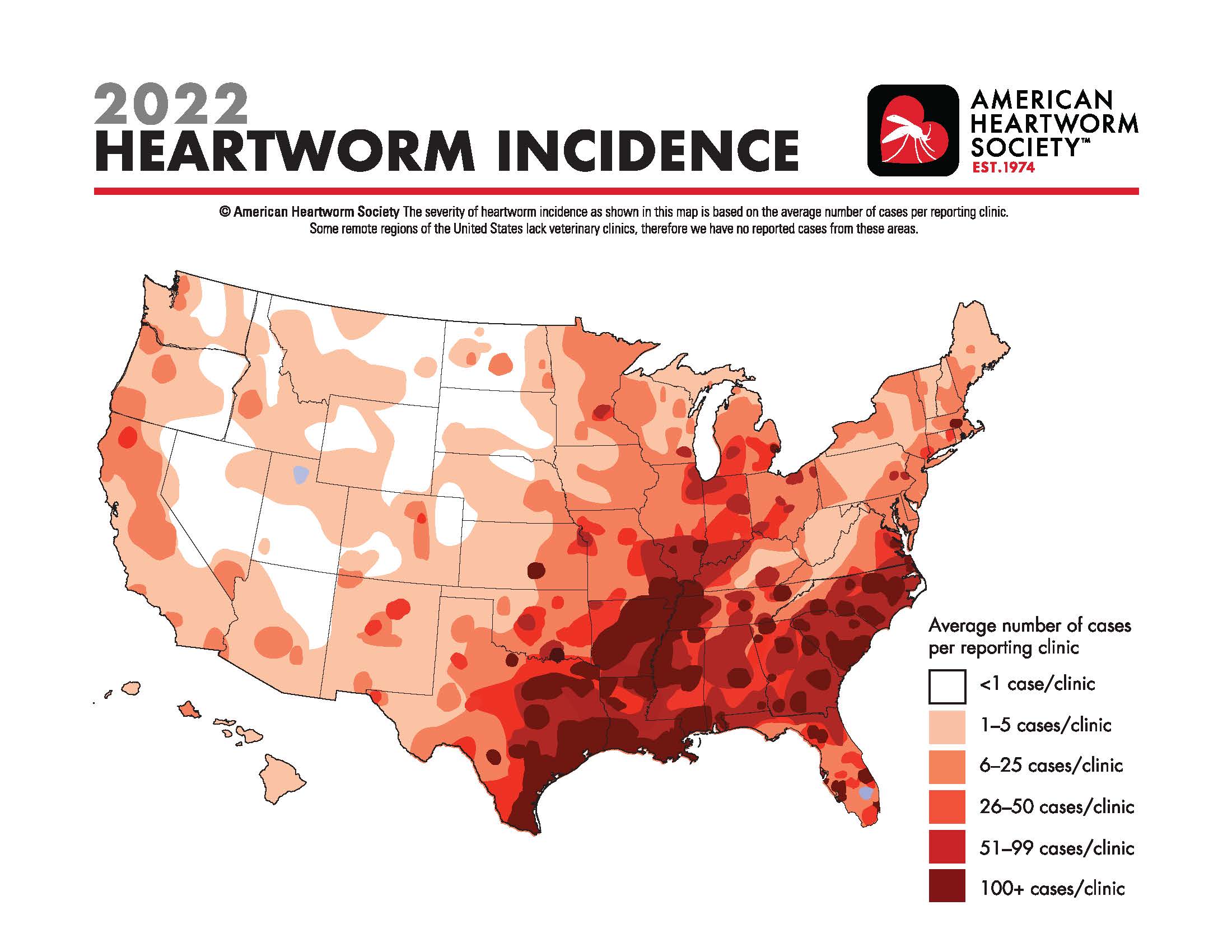
Heartworm Incidence Map
CLICK HERE TO SEE THE MAP at the American Heartworm Society
Catalyzing the field of canine comparative oncology, benefiting researchers far and wide

The Comparative Oncology Program at the National Institutes of Health is celebrating its 20th anniversary of advancing the study of cancer in dogs to help canine and human patients. AVMA News spoke with the founding and current directors of the program and two other veterinarians in the field of canine comparative oncology about their work and the importance of the program. This is the third article in a three-part series.
By Katie Burns
March 20, 2023
The Comparative Oncology Program at the National Institutes of Health has transformed canine comparative oncology since the program’s founding 20 years ago, according to Dr. Deborah W. Knapp at Purdue University and Dr. Steven Dow at Colorado State University, two of many veterinarians working in the field.
Helping pets and people
Dr. Knapp directs the Werling Comparative Oncology Research Center at Purdue University College of Veterinary Medicine and serves on the steering committee for the NIH-funded Integrated Canine Data Commons. Purdue’s program in canine comparative oncology was formed back in 1979 and has participated in the Comparative Oncology Program at the NIH since the start.

Dr. Knapp began her career working in a small animal practice, where she observed anti-cancer effects in dogs on piroxicam, a nonsteroidal anti-inflammatory drug. She studied the topic during her residency in veterinary oncology at Purdue. She later joined the Purdue veterinary faculty, and her research has focused on bladder cancer in dogs—which responds strongly to piroxicam.
Furthermore, bladder cancer in dogs is similar to muscle-invasive bladder cancer in humans. Now piroxicam is widely used in canine oncology, and there have been studies in human medicine of drugs in that class.
“I love the opportunity to help people with their pets when I know how incredibly important that is, and you form those bonds with the owners, and you’re helping their animals,” Dr. Knapp said. “And then at the same time, you’re generating information that can help human cancer patients. And for me, that’s a very special opportunity to have.”
Dr. Knapp said the Comparative Oncology Program at the NIH catalyzed the whole field—giving legitimacy to it, bringing in funding, and coordinating efforts.
Recently, Dr. Knapp and her team finished a study on early detection of bladder cancer in Scottish Terriers, with the results published by Frontiers in Oncology in November 2022. She said, “By the time we see animals with cancer, which is very similar to when physicians see people with cancer, the cancer can be pretty advanced before the diagnosis is even made.”
Scottish Terriers are at high risk of bladder cancer. The team followed 120 dogs that were at least 6 years old at the start of the study, screening them every six months for three years, and found bladder cancer in 32 of the dogs before any outward evidence of cancer. Treatment with deracoxib, another NSAID, was much more effective after finding the cancer early.
Old and new
Dr. Dow, a professor of clinical sciences at Colorado State University College of Veterinary Medicine & Biomedical Sciences, got involved with the Comparative Oncology Program at the NIH years ago when CSU was one of the sites running immunological assays in support of several studies through the program’s Comparative Oncology Trials Consortium.

Dr. Dow’s focus is developing immunotherapies for dogs with cancer. He participated in the first round of the PRE-medical Cancer Immunotherapy Network Canine Trials. The NIH funded PRECINCT first in 2017 and again at the end of 2022. Dr. Dow’s laboratory repurposes older drugs designed for other diseases, such as medications for hypertension that have immunological properties that make them promising for cancer treatment.
A recent study out of the laboratory found that using losartan, a medication for hypertension, combined with toceranib, a cancer drug, resulted in tumor stabilization or regression in half of dogs with advanced relapsed metastatic osteosarcoma to the lungs. The results of the osteosarcoma research were published in Clinical Cancer Research in February 2022.
The laboratory also studies other drug combinations that could be used in veterinary clinics now. Dr. Dow said: “These drugs, they’ve been around for a long time. They’re generic, the cost is affordable, and they have good safety margins.”
Malignant gliomas are aggressive brain tumors that share similarities between dogs and humans. A second study from Dr. Dow’s laboratory, published in Cancer Research Communications in December 2022, found that the combination of losartan and propranolol, a beta blocker, along with a cancer vaccine induced durable tumor responses in eight of 10 dogs with gliomas.
Dr. Dow said he thinks the biggest impact of the Comparative Oncology Program over the past two decades has been to increase the visibility of dogs with cancer as a translational model for humans with cancer, benefiting researchers whether or not they work directly with the program.
The role of the program has been not only creating networks, he said, “but also stimulating these interest groups that really begin to think deeply about cancer in dogs and how it applies to similar cancers in humans.”
The Troublesome Cushing’s Syndrome
March 31, 2023 / General Health / By Hemopet https://hemopet.org/the-troublesome-cushings-syndrome/?utm_source=Klaviyo&utm_medium=campaign&_kx=qjTvDeFUAmu9T1-bVDHL1OrzQOTI-Sa8jw_Kf-MGhbY%3D.Ypvfhc

Cushing’s syndrome in dogs is complex, difficult to diagnose, and tricky to treat. Before we get into all of that, we need to review the mechanisms that may cause it.
The Physiological Mechanisms
The pituitary gland is located in the brain. The adrenal glands lie near the kidneys. The pituitary gland tells the adrenal glands what to do.
How does the pituitary gland do this? Well, it releases a chemical called adrenocorticotropic hormone (ACTH). ACTH then stimulates the adrenal glands to release another hormone called cortisol, which is commonly known as the “flight or fight” stress hormone.
When the Pituitary-Adrenal Connection Goes Awry
Pituitary-Dependent (PDH) – If the pituitary gland develops a tumor that is most often benign, it will overproduce and release more ACTH. This overproduction of ACTH causes the adrenal glands to overproduce and release more cortisol. Once the pituitary gland realizes that there is an excess of cortisol circulating in the body, it will then underproduce ACTH. This form of Cushing’s disease accounts for 80-85% of the cases in dogs.
Adrenal-Dependent (ADH) – More rarely, an adrenal gland can develop a tumor that may be cancerous. This, too, can cause the release of excessive amounts of cortisol and suppresses the release of ACTH.
Drug-Related – Oral or injectable prescription glucocorticoid steroids (a class of corticosteroids) can cause another form of Cushing’s syndrome, termed “iatrogenic Cushing’s syndrome” . They suppress the adrenal glands by adding extra cortisol to help fight skin or inflammatory conditions. When given in excessive amounts or over a long period of time, they can cause the iatrogenic Cushing’s syndrome.
Atypical Cushing’s – In dogs with atypical Cushing’s syndrome due to a problem with the pituitary gland or ADH , we can observe enlargement of the liver, liver pathology, and bilaterally enlarged adrenal glands are usually present. An increased endogenous ACTH level is seen, along with the usual clinical signs, blood work results and hair coat problems. The other adrenal gland can be atrophied (shrunken). There is a decreased endogenous ACTH level and the usual clinical signs, blood work results and hair coat problems. This form of Cushing’s syndrome can be more difficult to diagnose and measurement of 17-Hyroxy (17-OHP) progesterone before and after giving ACTH is often required (see more below).
Wait! I thought it was called Cushing’s disease?
Cushing’s disease is a form of Cushing’s syndrome and specifically refers to those with PDH tumors. Cushing’s syndrome is the general state of excessive levels of cortisol in the blood. In any event, the medical term for high levels of cortisol circulating in the blood is hyperadrenocorticism.
Signs of Cushing’s Syndrome
The most telltale sign of Cushing’s syndrome is a pot-bellied appearance. Additional signs are panting, dark spots, bladder infections, thin hair and/or skin, fat pads, excessive drinking and eating, and excessive amounts of calcium deposits in the skin (calcinosis cutis/skin mineralization).
This constellation of Cushing’s signs are called Cushingoid.
Diagnosing Cushing’s Syndrome
We can analogize the current diagnostics for Cushing’s syndrome with shopping for a couch. Have you ever gone couch shopping and you like certain features from different couches, but nothing’s perfect? For instance, you like the cushions on one model, but detest the armrests? Or, you like the armrests on another, but it has an upholstered skirt that you don’t like? Let’s not even get into the length, height, depth, fabric, patterns or colors!
Anyway, Cushing’s diagnostics are similar to the variety of couches: there are a lot of options, nothing’s perfect and all of it costs a bundle. But, unlike a couch, you cannot customize the diagnostics.
This is not to negate Cushing’s testing. Indeed, you need to have positive confirmation of Cushing’s syndrome and the location of the problem (pituitary or adrenal) before medicating.
Urinary Cortisol to Creatinine Ratio (UCCR) – This test is used as a pre-screening tool to rule out Cushing’s syndrome by measuring the first morning urine at home. However, stress can cause this number to fluctuate greatly, which is why you need to collect your pet’s urine at home (one teaspoon is enough in a clean plastic dish) when he first gets up and has not exercised, and then take it into your veterinarian to run this test. Even if it is negative, and the veterinarian still highly suspects Cushing’s syndrome, further testing is necessary.
Ultrasound – An abdominal ultrasound helps by pointing us in the right direction. With PDH, both adrenal glands are abnormally enlarged. Whereas ADH, only one adrenal gland is enlarged and the other is small or atrophied.
ACTH Stimulation Test – If any dog has been given steroids in the past, this is the test experts want to use to diagnose iatrogenic Cushing’s syndrome. However, ACTH stimulation has a sensitivity of only 60%-85% (percentage of true positives), and a specificity 60%-93% (percentage of true false negatives). Additionally, it does not indicate the location causing the Cushing’s syndrome.
If this is the chosen test, it is wise to concurrently analyze 17-Hydroxyprogesterone (17-OHP) concentrations in response to ACTH administration. Dogs with atypical Cushing’s disease have an exaggerated 17-OHP response to ACTH. Other dogs with Cushing’s syndrome could have deranged steroid production pathways, such that certain steroid precursors may be abnormally increased and responsible for the presenting clinical signs, whereas cortisol concentrations are normal.
By the way, diagnosis of atypical Cushing’s disease may also include measurement of: androstenedione, estradiol, progesterone and aldosterone.
Low Dose Dexamethasone Suppression Test (LDDS) – This is considered the gold standard for testing for Cushing’s syndrome at this time unless iatrogenic Cushing’s disease is suspected. It can distinguish between PDH and ADH. The sensitivity is good at 95%, but the specificity is poor and only 50%-75%.
Endogenous ACTH (eACTH) – Endogenous ACTH should not be used to diagnose Cushing’s disease, but will help with location and secondary confirmation. The sample has to be prepared properly at the veterinarian’s office to ensure stability, then frozen, and sent frozen to a veterinary reference laboratory. Due to all of these handling factors, it is really not an ideal test unless the blood collection is at a research institution.
Zomedica has developed an in-house, point-of-care diagnostic machine that measures eACTH using bulk acoustic wave technology. (This is not an endorsement; we simply want you to know your options.) An LDDS test or ACTH will still need to be conducted.
Options to Treat Cushing’s Syndrome
If Cushing’s syndrome is confirmed, veterinarians have only a handful of treatment options. In fact, many veterinarians choose not to medicate for the disease based on bloodwork, other currently prescribed medications, additional conditions, and potential side effects of the Cushing’s disease medications.
Surgery – If it is ADH, surgical removal of the tumor is possible but can be very difficult, especially if it has spread. However, due to the complexity of removal, most cases are treated with medication.
Trilostane (Vetoryl) – At this time, this is the only prescription medication approved by the Food and Drug Administration (FDA) to treat both PDH and ADH. Trilostane works by stopping the production of cortisol in the adrenal glands. However, it should not be given to a dog that takes certain medications for heart disease, is pregnant, and/or has kidney or liver disease. Additionally, the ACTH stimulation test is preferred to monitor trilostane therapy. Return of clinical signs of Cushing’s disease can occur in some dogs while still on trilostane.
Common side effects are poor or reduced appetite, vomiting, lack of energy, diarrhea, and weakness. More serious (but considered rare) side effects include bloody diarrhea, collapse, severe sodium/potassium imbalance, and destruction of the adrenal gland that may result in death.
Selegiline (Anipryl) – Selegiline is an monoamine oxidase inhibitor (MAOI), and is also FDA approved, but only for uncomplicated PDH. It should not be given to dogs that take other MAOIs, meperidine, tramadol, tricyclic antidepressants, selective serotonin reuptake inhibitors, or alpha-2 agonists.
Side effects include vomiting, diarrhea, restlessness, disorientation/confusion, aggression, repetitive movements, tiredness, drooling, itchiness, licking, trembling, and lack of appetite. Rare, but serious side effects, include deafness and panting more than usual.
Mitotane (Lysodren) – Mitotane is a human chemotherapy drug that veterinarians can prescribe “off-label” to treat Cushing’s disease. It works by destroying the layers of the adrenal gland that produce cortisol. It should be used cautiously in pets with diabetes mellitus or kidney or liver disease. The following medications should be used with caution when given with mitotane: central nervous system (CNS) depressant drugs, fentanyl, insulin, midazolam, phenobarbital, selegiline, spironolactone, or warfarin.
Common side effects are decreased appetite, vomiting and diarrhea. Other side effects include lethargy, incoordination, weakness, or yellowing of the skin, gums, or whites of the eyes.
Regular monitoring of cortisol levels is required.
Melatonin – The enzymes that are typically elevated in HAC are inhibited by melatonin. Also, in dogs with adrenal disease treated with melatonin, repeat adrenal steroid panels show that cortisol levels are consistently reduced. Melatonin treatment for cases of mild to moderate canine adrenal disease can be effective, and particularly in cases where adrenal sex steroids are increased.
Melatonin plus phytoestrogens – Melatonin given in combination with phytoestrogens (isoflavones, lignans, and genistein) is known to inhibit adrenal steroid production. Combinations of melatonin and phytoestrogens, especially the SDG flax hull or HMR Norwegian spruce lignans have proven increased efficacy in treating these conditions.
References
“Adrenal Function Testing.” The College of Veterinary Medicine at Michigan State University, Michigan State University, https://cvm.msu.edu/vdl/laboratory-sections/endocrinology/adrenal-function-testing.
Behrend, E N et al. “Diagnosis of spontaneous canine hyperadrenocorticism: 2012 ACVIM consensus statement (small animal).” Journal of veterinary internal medicine vol. 27,6 (2013): 1292-304. doi:10.1111/jvim.12192, https://onlinelibrary.wiley.com/doi/full/10.1111/jvim.12192.
Dodds, W. Jean. “Diagnosing Atypical Cushing’s Disease/Syndrome in Dogs.” Dr. Jean Dodds’ Pet Health Resource, Tumblr, 17 Apr. 2016, https://drjeandoddspethealthresource.tumblr.com/post/142960916541/atypical-cushings-dog#.Y6CxAXbMLIW.
“Treating Cushing’s Disease in Dogs.” U.S. Food and Drug Administration, FDA, 8 July 2021, https://www.fda.gov/consumers/consumer-updates/treating-cushings-disease-dogs.
A dog died after getting bird flu in Canada. Here’s how to keep your pets safe.
See the video here: https://www.usatoday.com/story/news/health/2023/04/05/dog-dies-bird-flu-how-to-keep-pets-safe/11607516002/
Adrianna Rodriguez USA TODAY
A pet dog has died after testing positive for the highly contagious bird flu in Ontario, Canada, health officials said this week.
The Canadian Food Inspection Agency said the dog tested positive for the virus on Saturday after chewing on a wild goose. The dog subsequently developed clinical signs and died.
While further testing is underway, a necropsy showed its respiratory system may have been compromised by the virus, according to Tuesday’s statement.
Canadian health officials say it’s the first case of its kind reported in the country. The American Veterinary Medical Association says only a few cases of bird flu in cats or dogs have been reported worldwide, with none occurring in the United States.While the U.S. Department of Agriculture hasn’t reported any cases among pets, the agency has found cases in other mammals like skunks, raccoons, mountain lions, bears and foxes. Canadian health officials say it’s the first case of its kind reported in the country. The American Veterinary Medical Association says only a few cases of bird flu in cats or dogs have been reported worldwide, with none occurring in the United States.
While the U.S. Department of Agriculture hasn’t reported any cases among pets, the agency has found cases in other mammals like skunks, raccoons, mountain lions, bears and foxes.
How to keep your pet safe from bird flu
Canadian and U.S. health officials say pets’ risk of contracting and dying from bird flu appears to be very low – but not zero.
Here’s what you can do to keep your pet safe from bird flu:
►Don’t feed pets, including dogs or cats, raw meat from game birds or poultry.
►Keep pets away from dead wild birds found outside.
►Contact a veterinarian if your pet develops symptoms including fever, lethargy, lack of appetite, difficulty breathing, tremors or seizures, or conjunctivitis.
“Words Matter” – The Whole Dog Journal
Why the language you use makes a difference in your relationship with your dog – and perhaps even the success of your training program.
By Pat Miller, CBCC-KA, CPDT-KA

I’ve been training dogs professionally for 27 years, but I don’t use “commands” for this purpose, I use “cues.” What difference does it make? A lot!
The definition of command is “an authoritative order.” Even when we use gentle training methods, if we think “commands,” our brains connect to the authoritative definition and we are likely speak in a louder, harsher (commanding!) tone of voice. In contrast, a cue is an invitation to perform a behavior for which your dog can be reinforced with a treat, play, praise, or the opportunity to perform a behavior the dog enjoys. We are far more likely to speak softly and gently when we use “cues.”
Words to avoid
“Command” is just one of many words that we force-free trainers avoid. Here are others that interfere with the message of kindness and mutual respect we want to send to our dogs:
- “It.” This word is used to refer to non-living objects. Dogs (and other animals) are living, thinking, feeling beings. Use he, she, him, and her rather than “it” when referring to a dog. When you acknowledge the sentience of non-human animals, you’re likely to treat them better.
- “Breaking.” Breaking evokes force, and we’re not “breaking” anything, we’re “training” – so we use housetraining (not housebreaking) and say we are training desirable behaviors (not breaking bad habits).
- “Obedience.” We want a partnership with our dogs – a happy willingness to offer behaviors we ask for, not their submission to our authority. That’s why we offer good manners training or family dog training rather than “obedience classes.”
- “Make.” We don’t “make” our dogs do things. “Make” suggests force and coercion. Instead, we ask our dogs for certain behaviors, invite them, help them, and encourage them.
- “Bad.” Dogs aren’t bad and they don’t do bad things – though occasionally they may do something inappropriate. When we think of them as bad, we give ourselves tacit permission to punish them. But when we frame their behavior as “inappropriate,” we’re more likely to think in terms of management and teaching appropriate behaviors rather than punishment.
- More pejoratives. I cringe when someone refers to a dog as stupid, stubborn, disobedient, or any other negative adjectives, placing the blame for any unwanted behavior directly on the dog’s shoulders. When a dog doesn’t do what you ask, it’s because she can’t for some reason: she doesn’t understand, she’s too stressed, was distracted, didn’t hear you, is in pain or otherwise physically unable, you haven’t made the consequence of the behavior reinforcing enough, or you haven’t generalized it well (you haven’t trained her!). Figure out why she can’t do it and then help her succeed.
Respectful language
Think carefully about the words you and/or your instructor use to discuss training and your dog. Philosopher and cognitive scientist Daniel Dennett suggests that language lays down the tracks upon which thoughts can travel. Your words connect to your thoughts and influence your behavior. If your words align with your philosophy of creating a kind and nurturing relationship with your dog based on mutual trust and respect, you’re likely to behave accordingly – and you and your dog will be well on your way to achieving that pinnacle.
WDJ’s Training Editor Pat Miller, CBCC-KA, CPDT-KA, grew up in a family that was blessed with lots of animal companions: dogs, cats, horses, rabbits, goats, and more, and has maintained that model ever since. She spent the first 20 years of her professional life working at the Marin Humane Society in Marin County, California, for most of that time as a humane officer and director of operations. She continually studied the art and science of dog training and behavior during that time, and in 1996, left MHS to start her own training and behavior business, Peaceable Paws. Pat has earned a number of titles from various training organizations, including Certified Behavior Consultant Canine-Knowledge Assessed (CBCC-KA) and Certified Professional Dog Trainer – Knowledge Assessed (CPDT-KA). She also founded Peaceable Paws Academies for teaching and credentialing dog training and behavior professionals, who can earn “Pat Miller Certified Trainer” certifications. She and her husband Paul and an ever-changing number of dogs, horses, and other animal companions live on their 80-acre farm in Fairplay, Maryland.

