Getting to the root cause of pet’s increased drinking and urinating
When an owner asks why a pet is constantly drinking water and urinating more frequently, veterinarian Robert Runde explains the potential conditions that could lead to the symptoms in dogs and cats, discusses tests used to help discern the cause and points out the health consequences in pets who are not diagnosed and treated. Dr. Runde emphasizes the importance of promptly seeing a veterinarian for any animal whose drinking and urinating habits have increased. TCPalm.com (Fort Pierce, Fla.)
Question: Why is my dog drinking and urinating more? Is this normal? What is the quickest way to find out the causes?
Answer: One of the most common owner complaints in veterinary medicine for both cats and dogs is for increased drinking and urination. There are a plethora of causes, but if your animal shows these clinical signs a timely appointment with your veterinarian is warranted. You may notice that your pet has increased frequency and volume of drinking/urination, is having “accidents” in the house, is showing signs of urinary incontinence (waking up in a pool of urine, dribbling urine while walking around), or urinating in unusual places.
Some of the common causes of increased drinking and urination in dogs are diabetes mellitus, kidney disease, infection in the urinary tract, excessive adrenal hormone production, pyometra (infection of the uterus), and liver disease. In cats, the most common causes of increased drinking and urination differ slightly than of those in dogs, and include kidney disease, diabetes mellitus, hyperthyroidism, and liver disease. Most of these potentially life-threatening conditions can be quickly ruled out through accurate history taking, a thorough physical examination, and simple blood and urine tests. In some cases additional diagnostics may need to be performed. These may include X-rays of the chest and abdomen, cultures and hormonal blood tests. Depending on the results of the diagnostics referral to an iternal mdicine specialist may be helpful as more advanced diagnostics/treatments may be required. These could include ultrasound, Xrays with contrast, endoscopy, MRI and hyperbaric oxygen therapy.
For example, if diabetes mellitus is left untreated, severe metabolic disturbance (Ketoacidosis) will develop. This is a life-hreatening condition requiring 24-our intensive care.
An infected uterus occurring in female intact dogs requires an emergency surgery. If not addressed promptly, this condition may prove fatal.
Untreated hyperthyroidism in cats can result in severe weight loss, chronic diarrhea/vomiting and significant heart disease. Hyperthyroidism may be managed medically, or more definitively treated with radioactive iodine (I-131) therapy.
There are a variety of liver conditions often require more advanced diagnostics such as ultrasound, full thickness biopsies, or a portogram (videofluoroscopy). Untreated liver diseases may progress to cirrhosis (irreversible scarring of the liver).
Hyperadrenocorticism is a condition of excessive adrenal hormone production. Although a diagnosis in most cases is relatively easy to obtain, some specific cases require further diagnostics such as an abdominal ultrasound to evaluate the adrenal glands and liver, and an MRI to evaluate the pituitary region of the brain.
Prompt identification of the cause of increased drinking/urination leads to a better chance of successful outcome. If you notice any increased drinking and/or urination in your pet please contact your primary care veterinarian immediately.
Robert Runde, VMD
Owners and veterinarians concur: Preventive care is the best care
 Owners and veterinarians are similarly focused on preventive care, including vaccinations and parasite control, writes veterinarian Ann Hohenhaus, who discusses the results of a survey. Owners expressed concern over pet medication costs, but Dr. Hohenhaus endorses veterinary-grade medications, noting the medications are specifically designed for animals. WebMD/Tales from the Pet Clinic blog
Owners and veterinarians are similarly focused on preventive care, including vaccinations and parasite control, writes veterinarian Ann Hohenhaus, who discusses the results of a survey. Owners expressed concern over pet medication costs, but Dr. Hohenhaus endorses veterinary-grade medications, noting the medications are specifically designed for animals. WebMD/Tales from the Pet Clinic blog
By Ann Hohenhaus, DVM
Pet owners said they were primarily concerned with vaccinations, fleas and ticks, heartworms, intestinal parasites, and spending money on medications. This list appears to overlap with the veterinary list on the topic of intestinal parasites, and both owners and vets are squarely focused on preventive healthcare; care to keep their favorite furry, feathery, or scaly companion healthy.
Vaccinations
Vaccinations float to the top of most pet owners’ lists because they save pets’ lives. Before vaccinations were available for common diseases like canine distemper and feline panleukopenia, these diseases spread through neighborhoods like wildfire, often resulting in the deaths of many pets. Decreases in the recommended frequency of some vaccines, coupled with the association between injections and tumors, has raised many questions in pet owners’ minds.
Intestinal parasites
Both pet owners and veterinarians agreed intestinal parasite control was an important issue for pets. How could it not be? Intestinal parasites are high in yuck factor, high in pet discomfort, and on the list of diseases people and pets can share.
Fleas and ticks
These critters are very similar to intestinal parasites with regard to yuck factor and pet discomfort. A pet with a flea infestation may mean you also have a house or apartment with a flea infestation since fleas spend more time off your pet than on. Pet owners want to avoid an expensive exterminator bill by preventing fleas on their pet. Pet owners also want to prevent fleas and ticks to protect their pet against diseases like Lyme disease and blood parasites.
Heartworms
Because heartworms are a serious health concern in both dogs and cats, they are an important medical issue for most pet owners. Nearly every state in the United States reports cases of heartworm in resident dogs and cats. This map shows heartworm cases by state.
Year-round heartworm preventative is a “two-fer” since most prevent both heartworms and some intestinal parasites.
Pet medications
Pet owners want the best for their pet. In my mind, the best are veterinary-specific products. I prefer to prescribe medications developed specifically for veterinary patients rather than human or compounded medications. Veterinary-specific medications assure you, the pet owner, the product has been tested in dogs or cats and will be absorbed, metabolized, and effective in your pet. But, because most pets do not have insurance and medications are paid for “out of pocket,” many times pet owners can be surprised at the cost. As a pet owner myself, I believe that these veterinary-specific medications are worth paying for.
After looking carefully at the two lists of pet healthcare issues, one from pet owners and the other from veterinarians, are they really so different? Both groups’ lists really have only one item and it’s the same one: healthy, happy pets.
Why cats don’t make it to the veterinarian’s office enough
 More dogs get regular veterinary care than cats, writes veterinarian Barry Burtis. He suggests many factors contribute, including cats’ general aversion to traveling in carriers, owners’ mistaken belief that indoor cats don’t need regular veterinary care and the feline ability to mask symptoms. Dr. Burtis emphasizes the connection between regular veterinary care and optimum health for cats. The Burlington Post (Ontario) (11/29)
More dogs get regular veterinary care than cats, writes veterinarian Barry Burtis. He suggests many factors contribute, including cats’ general aversion to traveling in carriers, owners’ mistaken belief that indoor cats don’t need regular veterinary care and the feline ability to mask symptoms. Dr. Burtis emphasizes the connection between regular veterinary care and optimum health for cats. The Burlington Post (Ontario) (11/29)
Statistics tell us that dogs visit veterinarians much more regularly than cats. On the other hand, polls tell us both dog and cat owners equally recognize the value of veterinary care for their pets.
So, why the disconnect? Why do you suppose dogs average 1.8 veterinary visits per year while cats get to see us only 0.7 times a year? Are dogs or their owners just hypochondriacs, excessively worried or anxious about illness and health? Are dogs just wimps — limping, whining and crying with every little ailment? Do dog owners just have huge amounts of money they wish to use supporting veterinary medicine? Do cat owners not love their feline as much as dog owners care for their dog? Are cats more resistant to disease, requiring less vaccination protection or other healthcare advice?
In my opinion, none of the above offers a correct explanation for the difference. No, there are other much more likely reasons.
Here are some that come to mind. Cats are homebodies. Getting into a carrier, in the first place, is not a happy experience for many cats, neither is it fun for their owner. No matter how smooth the ride, few cats love to go in the car. The yowling, scratching and sometimes bad odours emanating from the cat carrier can take the pleasure out of the ride for the cat’s car companions, as well. At the veterinary hospital, the cat’s attitude toward the cat carrier usually suddenly changes. It’s the nearest thing to home in that place. Why would they want to come out and be weighed, poked, prodded or needled? No, when a cat fails to see any benefit or value associated with this experience, their behaviour reflects their concerns. Is there anything to make the experience more pleasant for all? Well, as a start, begin at a very early age and continue through their life to build a better relationship between a kitten/cat and its carrier. Bring it out of storage at times other than just before a stressful car ride. That should make the trip a bit easier. Then it’s going to be up to the owner to realize most everyone experiences a bit of stress when they go to see their doctor.
People sometimes mistakenly believe that because their cat stays inside it really does not need the benefit of vaccinations. I believe this is another reason cats fail to get to see their doctor as often as they should. However, municipal bylaws mandate that all cats — regardless of lifestyle — must be vaccinated against rabies. Panleukopenia, feline leukemia and the respiratory viruses — rhinotracheitis and calici virus — are all diseases that can be protected against. A veterinarian should determine which ones are necessary for an individual cat.
Do some cat owners just believe it’s too expensive to visit a veterinarian? People are usually thrilled to learn about the medicines, treatments and therapies that are available for their pets these days. Especially now with the availability of pet health insurance, I hope not many cats are failing to get the full benefits of healthcare because of cost.
A perhaps more legitimate reasons for cats and veterinarians not getting together as often as they should is that cats mask their illnesses very well. Cats are predators, but they are also a prey species. In the wild, showing weakness is the best way to hasten your decline. Cats often hide even severe arthritis, because they are moving around usually much less than dogs. Using the privacy of a litter box, instead of urinating on a walk like a dog, means cat owners are probably much less aware of volumes of urine a cat is producing, behaviour when a cat is urinating or the appearance of a cat’s urine. Lumps and bumps on a cat’s body surface may be less quickly spotted than with a dog. When a cat vomits, is it just a hairball or is it vomiting for some other reason and the hair just happens to be brought up as an effect, but not the cause of the problem?
How do we make cats equal opportunity users, with dogs, of today’s healthcare for pets? It’s very easy. Just make sure your cat visits its veterinarian at least once per year. It can receive a general physical examination, be updated on vaccine needs, get reliable, current diet and healthcare advice, all with a minimum of stress and expense.
Funeral home offers services for 4-legged family members
 D.O. McComb & Sons’ Tribute Center in Indiana includes services for deceased pets such as burial, cremation and a private room for viewing by owners, reflecting pets’ modern status in many homes as family members.
D.O. McComb & Sons’ Tribute Center in Indiana includes services for deceased pets such as burial, cremation and a private room for viewing by owners, reflecting pets’ modern status in many homes as family members.
Memorials to pets prove it’s more than puppy love
An unusual item appeared in the newspaper the other day. It was an obituary – for a dog.
The death notice identified the dog’s owner and even included calling hours at D.O. McComb & Sons new Tribute Center on West Main Street near Lindenwood Cemetery.
While the obituary was, as far as I can recall, a first for the newspaper, the concept of special treatment for a deceased pet is nothing new.
People have been falling in love with their pets since long before Rin Tin Tin, Lassie or Old Yeller came along, sometimes with good reason. A pet will never tell you you’re ugly or overweight, and it will never ask you where you’ve been when you come home late. It will just be delighted to see you.
While your kids may prove to be crushing disappointments, a pet generally doesn’t have the wherewithal to ruin the family name, get busted for selling drugs or sell your jewelry while you’re out of town.
Truth be told, for many people, a pet is the most loyal – even the only truly loyal – creature in their lives.
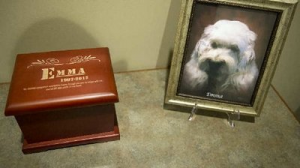
That has become evident to the people at D.O. McComb. A lot of people want a respectful exit for their pets, so when the funeral home opened the Tribute Center in October it included something unusual: a separate crematorium for pets, and a separate room, now called Emma’s Room, where a deceased pet can be briefly laid out and the owner can enter and say hello and offer one last goodbye before cremation, Dave McComb says.
It’s just a sign of the times, he said. Pets have become more important as members of the traditional family move to far-flung places. Kids leave. Wives leave. But pets remain as faithful companions and, McComb said, their status has become elevated.
Other animals, such as service dogs and police dogs, have earned a higher status in the minds of many. Maybe they don’t rate a funeral, but a thoughtful sendoff is soothing for the owners.
McComb’s can either cremate a pet and put its ashes in an urn, or arrange a burial in a portion of Riverview Cemetery that has been set aside for pets.
The funeral home hasn’t promoted the service yet, but at a Tribute Center open house, the concept drew a lot of attention and was well received, McComb said.
“We’ve had requests for even services for a while now,” McComb said.
While you won’t find preachers conducting funerals (don’t all dogs go to heaven anyway?) there can be services where an owner or friend might even eulogize an animal and friends or family members can show up and offer condolences.
“What we’ve learned is that people fall into two categories: pet owners and pet parents.”
To the pet parent, a pet becomes just as important as any other member of the family, somebody they will always remember.
The cost of a pet cremation? It varies depending on the size of the animal, which can obviously vary wildly, but the pet crematorium can handle animals up to 300 pounds.
Feline asthma: Diagnosis and treatment
 Asthma occurs when an allergen incites airway inflammation, resulting in varying levels of respiratory distress, more commonly in cats than in dogs, according to veterinarian Bernhard Pukay. Some cats experience mild symptoms such as coughing fits that resolve on their own, while others can have severe reactions that progress to panting and even death in rare cases, writes Dr. Pukay. X-rays help to make the diagnosis of asthma and rule out other conditions. Treatment depends on the severity of symptoms, according to Dr. Pukay, who points out that some cats may only need monitoring while others require medication.
Asthma occurs when an allergen incites airway inflammation, resulting in varying levels of respiratory distress, more commonly in cats than in dogs, according to veterinarian Bernhard Pukay. Some cats experience mild symptoms such as coughing fits that resolve on their own, while others can have severe reactions that progress to panting and even death in rare cases, writes Dr. Pukay. X-rays help to make the diagnosis of asthma and rule out other conditions. Treatment depends on the severity of symptoms, according to Dr. Pukay, who points out that some cats may only need monitoring while others require medication.
Question: We have a four-year-old calico cat. About three months ago, she started wheezing and having coughing spells. These episodes only last for a few minutes and then she seems perfectly normal afterward. She is still very active and appears healthy otherwise.
Our vet took chest X-rays and told us she had asthma. We were also told that medication was not really necessary at this time. Is this true? What are the chances that she will get worse and eventually need treatment? Could this kill her?
Answer: Your cat has a condition called Feline Asthma, which has several other names, including bronchial asthma, chronic bronchitis and allergic bronchitis. While it can be a problem in cats of all ages, it usually occurs most often in young and middle-aged cats. Dogs can also get asthma, but it is much more common in cats.
Put simply, asthma is an inflammation of the airways that is caused by an adverse reaction to allergens. Specifically, inhaled allergens cause a sudden contraction of the muscles around the windpipe and this leads to symptoms such as wheezing and coughing. It is usually difficult to determine precisely which allergens will trigger a reaction, but grass and tree pollens, house dust, smoke, sprays (hair sprays, deodorants, etc..) have been implicated.
Typically, a cat with a mild case of asthma will have a dry, hacking cough that may be confused with gagging, retching or vomiting. These cats will have episodes of coughing and wheezing, yet can be perfectly fine in between “attacks”.
In more severely affected cats, the coughing and wheezing may become a daily occurrence and they may experience breathing difficulties to such an extent that they start open-mouth breathing and panting. In a very small number of cases, feline asthma can be life threatening. In these cases, an injection of epinephrine may be necessary during a severe attack.
There are several other diseases that can mimic asthma. Heartworm disease, congestive heart failure, lung cancer and pneumonia can all show clinical signs similar to feline asthma. For this reason, veterinarians turn to diagnostic tools such as chest X-rays or ultrasound, blood tests (including heartworm testing) and tracheal and bronchial washings (i.e. taking cell samples by flushing the trachea and lungs).
Depending on degree of severity, treatment of feline asthma can range from simple monitoring to symptomatic relief of clinical signs. Medications such steroids, antihistamines, and bronchodilators are usually effective.
Corticosteroids are the most effective drugs for treating feline asthma because they reduce the inflammation in the windpipe and bronchi. Bronchodilators are also used in some cases because they help to open up the air passages to make breathing easier.
While there is no cure for feline asthma, fatalities are extremely rare. In patients where respiratory distress is not a manifestation and inflammation can be kept under control with medication, the prognosis for control of this disease is excellent. Unfortunately if inflammation cannot be controlled, lung damage can occur and the prognosis is more guarded.
Stop and think before giving a pet as a holiday gift, experts say
 While a puppy or kitten under the Christmas tree may seem like the quintessential holiday gift, experts warn that pets given as gifts don’t always have a happy ending. Veterinarian Mollie Hurley advises against surprising people with animals as gifts, as they may not be prepared for the commitment. Animal shelter educator Deeann Schaefer notes that recipients of pets may not be financially or emotionally prepared for the responsibilities and often end up surrendering those animals to already overburdened shelters.
While a puppy or kitten under the Christmas tree may seem like the quintessential holiday gift, experts warn that pets given as gifts don’t always have a happy ending. Veterinarian Mollie Hurley advises against surprising people with animals as gifts, as they may not be prepared for the commitment. Animal shelter educator Deeann Schaefer notes that recipients of pets may not be financially or emotionally prepared for the responsibilities and often end up surrendering those animals to already overburdened shelters.
While the excitement of surprising a loved one with an adorable puppy or kitten may be tempting, pets are not like a sweater or piece of jewelry that can be easily returned or re-gifted.
“Pet ownership is not an impulse to jump into,” Dr. Mollie Hurley, of Stack Veterinary Hospital in Onondaga, said. “And by not talking it over with the recipient or really thinking things through completely, (giving or receiving a pet as a gift) might not be as enjoyable as it could be.”
Companion animals may live for 15 years, and need life-long care in homes where they are loved and treated as members of the family.
“We see it a lot,” Deeann Schaefer, humane educator at Wanderers’ Rest Humane Association, an animal shelter in Canastota, said. “The person they’re giving the pet to may not have time for it, they may not be able to afford a pet, and some of them may not even want a pet at that particular time.”
While a pet given as a gift initially costs the person on the receiving end little or nothing, there is no such thing as a “free” animal.
A spread sheet at aspca.org listed first-year pet care cost estimates — not including the cost of purchasing the animal — ranging from $1,314 for a small dog to $1,843 for a large dog, and $1,035 for a cat. Of course, that’s just for the first year, and as animals age, their need for veterinary care may increase.
Schaefer said that too often gift animals end up in shelters, which are already filled with unwanted pets. Or worse, they may be neglected, abused or abandoned. She estimates the number of dogs and cats at Wanderers’ Rest increases by at least 10 to 15 percent after the holidays.
“People realize they may have bitten off more than they can chew,” Schaefer said. “We see a lot of kittens and cats coming into the shelter six months later, when the cuteness has worn off. Same thing with puppies, eight or nine months later. Suddenly, it’s not the cute roly-poly puppy that was underneath the Christmas tree, it’s a dog that’s chewing up your furniture.”
Hurley said adding a young animal to a household at this time of year presents special challenges.
“During the holidays there’s a lot of chaos, it’s a hectic time. People have a lot of things going on and may not be able to pay attention to the pet’s needs,” she said.
Hurley also cited the health risks of young animals ingesting ribbon and other holiday items, and added, “Taking a puppy outside every couple hours to get it potty trained in the winter is certainly not easy,” she said.
Schaefer said the phones are already ringing at Wanderers’ Rest. “We actually have people calling and asking us, ‘When are you getting your puppies in?’ like we’re Kmart or something,” she said.
Schaefer recommends, instead, giving a pet-themed gift basket and a gift certificate from a shelter, which would allow the recipient to personally pick out his or her own animal.
If a person says they want to adopt a dog or cat to give to someone else, Schaefer said Wanderers’ Rest requires the recipient to come in and confirm that he or she does indeed want the animal.
“Is it going to ruin the surprise? Yes, but we want every family member on board.” Schaefer said.
Costs of owning a pet include expenses for: Food and treats. Collars and leashes. Bedding. Veterinary care, including vaccines, medications, spaying and neutering, heartworm, flea and tick prevention. Grooming. Training, boarding or pet sitting. Fencing or containment systems. Time to exercise, play with and train the animal.
Fifi is helped by an Angel Fund Grant
The Portnoy family thanks the Northridge Pet Hospital for applying for and receiving a grant from AHF-SCVMA’s Angel Fund. Their domestic shorthair cat – Fifi – had an ulcerated growth between her paw pad and needed attention to several teeth. Fifi is recovering nicely.
Feline acne: Causes and treatment
 Feline acne, which is associated with overproductive sebaceous glands, usually appears on the chin, according to veterinarian Keeley McNeal. If the cat responds with rubbing and scratching, it can break the skin, causing a bacterial infection with draining skin pustules. If acne is caught early enough, applying topical benzoyl peroxide may clear it up, according to Dr. McNeal, but more advanced lesions require antibiotics, and she said it can be difficult to catch an early case of acne. “Cats can be pretty good at hiding it until they’re really miserable,” Dr. McNeal said.
Feline acne, which is associated with overproductive sebaceous glands, usually appears on the chin, according to veterinarian Keeley McNeal. If the cat responds with rubbing and scratching, it can break the skin, causing a bacterial infection with draining skin pustules. If acne is caught early enough, applying topical benzoyl peroxide may clear it up, according to Dr. McNeal, but more advanced lesions require antibiotics, and she said it can be difficult to catch an early case of acne. “Cats can be pretty good at hiding it until they’re really miserable,” Dr. McNeal said.
Because Smokey, 9, has such dark gray fur, his owner Nanette Goode of Joliet didn’t see the bumpy rash, but she could feel it.
So she researched his symptoms online and discovered Smokey had feline acne, which she treated with apple cider vinegar, as opposed to the traditional remedy of benzoyl peroxide.
“Getting a cat to comply with peroxide more than once is hard,” Goode said.
Within two weeks, Smokey’s acne had healed to a scab. Goode then eliminated what she believes caused the outbreak—his plastic food bowl—and replaced it with a stainless steel model.
“Bacteria can get in the scratches and grooves in the plastic,” Goode said, “and that can get on their skin when eating.”
Dr. Keeley McNeal at the Animal Care Center of Plainfield said feline acne often appears worse than it really is. It typically presents as little lumpy blackheads on a cat’s chin. Affected cats may look as if they’re stopped grooming themselves.
Feline acne is not breed specific, nor does it necessarily run in families, McNeal said. Certain cats may simply experience overactive sebaceous glands.
These glands produce a substance called “sebum,” which waterproofs hair and keeps skin supple. Allergic cats are at greater risk for developing it, possibly because their skin is already inflamed.
If the acne itches and the cat responds by rubbing, scratching and licking it, the chin may also become infected and painful. If the chin turns red and/or oozes pus, the acne will require antibiotic treatment. Otherwise only topic treatment with benzoyl peroxide wipes may be sufficient. Catching the acne before it reaches that point may be tricky.
“Cats can be pretty good at hiding it until they’re really miserable,” McNeal said.
The acne should heal in two to three weeks. If not, the cat might have an underlying condition (such as feline herpes, which can lower the immune system), a recent chin injury or another disorder.
For instance, indoor/outdoor cats that enjoy hunting can wind up with ulcers on their chins and lips from mites they pick up while eating mice. Infections that don’t clear up should be smeared under a microscope to rule out possible fungal infections. Certain skin parasites can also resemble feline acne.
Pale and white cats that like to lie out in the sun are especially prone to developing squamous cell cancer. An affected cat’s ears and lips will appear sunburned. A skin biopsy can detect the presence of skin cancer. See your veterinarian any time a wound does not heal.
Although feline acne is unsightly, cats cannot pass it onto humans or other cats in the household. There is also no way to prevent it, but feline acne will also not limit the cat’s day-to-day life or prevent it from participating in any special events.
And, unlike humans, cats won’t sit before a mirror brooding about what the other cats are thinking about their appearance.
“They can still go to prom,” McNeal said with a chuckle.
Scientists work to crack Lyme disease’s genetic code
Researchers at The University of Texas Health Science Center at Houston are working to identify the factors that explain the virulence of Borrelia burgdorferi, the spirochete that causes Lyme disease, which affects animals and an estimated 30,000 people in the U.S. per year. Using advanced technology, the team is testing the pathogen’s 1,739 genes in an effort to find the ones responsible for its ability to spread so readily. The findings are expected to help develop vaccines, diagnostic tools and treatments
ScienceDaily (Oct. 25, 2012) — Investigators at The University of Texas Health Science Center at Houston (UTHealth) have accelerated the search for the bacterial genes that make the Lyme disease bacterium so invasive and persistent. The discovery could advance the diagnosis and treatment of this disease, which affects an estimated 30,000 Americans each year.
Scientists hope to use this information to unravel the mystery of how the spiral-shaped bacterium Borrelia burgdorferi causes Lyme disease. Ticks carry the bacterium and transfer it to animals and humans when the tiny spider-like creatures bite. The Lyme disease microorganism was discovered in 1981.
“We believe that this will be one of the most significant publications in Lyme disease in the next several years. This global approach will help ‘move the field forward’ and also serve as a model for other pathogens with similar properties,” said Steven Norris, Ph.D., the study’s senior author and the vice chair for research in the Department of Pathology and Laboratory Medicine at the UTHealth Medical School.
The bacterium can invade almost any tissue in humans or animals and trigger an infection that lasts from months to years. Its symptoms include a reddish rash that often resembles a bull’s eye and flu-like symptoms. The disease can lead to nervous system problems, joint inflammation and heart abnormalities. Most instances of Lyme disease can be treated with antibiotics.
“Our long-term goals are to screen, identify and characterize the virulence determinants of the Lyme disease bacterium and thereby dissect the mechanism of pathogenesis in mammals and ticks,” said Tao Lin, D,V.M., the study’s lead author and assistant professor of pathology and laboratory medicine at the UTHealth Medical School. “With this information, we will have a clearer picture about the virulence determinants and virulence factors for this fascinating microorganism and the mechanism of pathogenesis behind this unique, invasive, persistent pathogen.”
Norris, the Robert Greer Professor of Biomedical Sciences at UTHealth, and Lin are running tests on the 1,739 genes in the bacterium to see which genes impact the microorganism’s ability to spread disease.
To do this, they mutated the bacterial genes and gauged the impact in a mouse infection model. Overall, 4,479 mutated bacteria were isolated and characterized. Whereas it took researchers about three decades to knock out less than 40 bacterial genes, Norris and Lin knocked out 790 genes in a comparatively short period of time; some genes were “hit” multiple times. A newly developed screening technique, which involves signature-tagged mutagenesis and Luminex®-based high-throughput screening technologies, can also be used to identify infection-related genes in other bacteria.
“This kind of study enables us to better understand the disease pathogenesis at the basic level,” said Charles Ericsson, M.D., head of clinical infectious diseases at the UTHealth Medical School. “In time, such understanding of virulence properties might enable us to develop vaccine candidates, better diagnostic tools and perhaps even targeted drug intervention.”
Norris and Lin are on the faculty of The University of Texas Graduate School of Biomedical Sciences at Houston.
Previously, Norris helped develop a method based on one of the bacterium’s proteins, called VlsE, for diagnosing Lyme disease. The test, which is now used worldwide, involves detection of VlsE-specific antibodies, which are often found in people and animals infected with Lyme disease.
Also participating in the study from UTHealth were Lihui Gao, D.V.M., Chuhua Zhang, Evelyn Odeh and Loic Coutte, Ph.D. Mary B. Jacobs and Mario Philipp, Ph.D., of the Tulane University Health Sciences Center collaborated on the study as did George Chaconas, Ph.D., of The University of Calgary in Canada. Mutated strains produced through this study are being made available to the scientific community through BEI Resources.
The study is titled “Analysis of an ordered comprehensive STM mutant library in infectious Borrelia burgdorferi: insights into the genes required for mouse infectivity.” The project described was supported by Award Number R01AI059048 from the National Institute of Allergy and Infectious Diseases.
Just like in people, allergies are a common occurrence in pets
 Allergic dogs are common visitors to veterinarian Brian Jenkins’ office, making up an estimated 20% of his clientele, and he can relate to their plight because he also suffers from allergies. The three categories of allergies in pets are flea allergy, food allergy and atopic dermatitis. While there is no definitive cure for allergic conditions, Dr. Jenkins says that with time and consistent treatment, many animals can experience relief from their symptoms.
Allergic dogs are common visitors to veterinarian Brian Jenkins’ office, making up an estimated 20% of his clientele, and he can relate to their plight because he also suffers from allergies. The three categories of allergies in pets are flea allergy, food allergy and atopic dermatitis. While there is no definitive cure for allergic conditions, Dr. Jenkins says that with time and consistent treatment, many animals can experience relief from their symptoms.
Nan Sterner could not figure out what was wrong with Sadie.
Since she was a puppy, the 4-year-old golden retriever and poodle mix – a goldendoodle – was constantly scratching.
“She was itching and scratching all the time,” Sterner said. “I thought it was fleas.”
But Sadie was found to be flea-free. She was still scratching, though, to the point where she had red and irritated patches of skin all over her body, and even had some scratched-open sores.
So Sterner brought Sadie to Aloha Animal Hospital in Hanover to find out what was wrong, and she was relieved to discover that her condition is treatable.
“Sadie has a huge amount of allergies,” said Dr. Brian Jenkins, veterinarian and co-owner of the animal hospital.
Some cats and dogs suffer from allergies, and often are allergic to the same things as people, like trees, grasses, weeds, and pollen, Jenkins said. While people usually suffer the effects of allergies through their respiratory systems, cats and dogs feel it in their skin.
And over the last year, with continuous warm and often wet weather, those allergies seem to be worse, and Jenkins is seeing more and more cases coming into his office all the time.
The good thing is while allergies are no fun, they are treatable.
Treating pet allergies
Even pets who have not shown signs of allergies before might be scratching their coats and looking for relief from the itching this year.
Jenkins said allergies have a threshold. An allergen might have no effect on a dog or cat in a normal year may flare up with more exposure.
Pets typically have three different kinds of allergies. One is a flea allergy, in which they have a reaction to flea saliva.
Along with common allergens, fleas have been thriving with weather conditions over the last year.
A second allergy is one that’s often difficult to diagnose, which is a food allergy. Most allergies start in the first few years, but food allergies can start at any time. Dogs are usually allergic to beef, followed by dairy and wheat. Cats are also allergic most to beef and dairy, as well as fish.
But the third and more common allergy, and the one Jenkins likes to study, is atopic dermatitis – or the skin allergy.
These allergies typically hit pets that are between 6 months and 3 years old. And they can be seasonal, caused by things like weeds, grass, mold or pollen, or they can be caused by things like dust that are present throughout the year. Tree pollens are particularly bad in Hanover this time of year, Jenkins said. And he said he is seeing lot of allergies to ragweed now, too, as well as sagebrush and a whole host of molds and spores.
“You won’t cure an allergy, but you can treat it,” Jenkins said.
One way to treat these is through the use of steroids, which is quick and cheap, but it can have negative side effects, such as ulcers, vomiting, diabetes and skin and coat problems.
Jenkins treats Sadie, and many of the pets he sees, with topical treatments for the skin, as well as allergy shots. It can be time consuming, and a financial commitment, but it’s often the best way to keep allergies under control, he said.
Every pet and each allergy is different, and Sadie is a pretty extreme case, too, suffering from a whole list of allergies, he said. But even with an extreme case like Sadie, and with the help of an owner who constantly monitors and applies medication, treatment can been successful, he said.
A doctor who understands
Allergies are not fun for pets. Or people. Jenkins takes a special interest in treating allergies because he has suffered from them since he was a little kid.
And as an allergy sufferer, he’s empathetic with what pets are going through when they come in his office with allergies.
He’s allergic to many of the same things as Sadie – particularly ragweed, which he said is vicious this time of year.
Like Sadie, he goes to his doctor for treatment, and is able to keep it under control.
Though he’s a general practitioner of veterinary medicine, and does not specialize in allergies, he takes a special interest in it. And with the hundreds of dogs and cats that come through his doors, he said he could open an allergy clinic if he wanted to. About 20 percent of the dogs he sees have some form of skin allergies.
Any breed is susceptible, he said, but allergies are particularly common among golden retrievers, labs, Boston terriers and shih tzus.
But there’s hope for all allergy sufferers.
“Dogs and cats are allergic to many of the same things as people,” Jenkins said. “And they can be treated in some of the same ways.”
While there is no silver bullet to treat all allergies, he said with time, patience, and constant treatment, allergies can be brought under control.
And dogs like Sadie can continue to live happy, itch-free lives


